Written by: Keara Kilbane, MD (NUEM ‘25) Edited by: Maren Leibowitz, MD (NEUM ‘23)
Expert Commentary by: Danielle M McCarthy, MD
Vagal Maneuvers Simplified
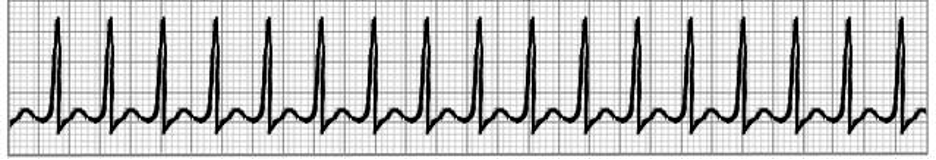
https://acls-algorithms.com/rhythms/supraventricular-tachycardia/
Introduction to Vagal Maneuvers:
Vagal maneuvers are considered the first line treatment for hemodynamically stable supraventricular tachycardia (SVT).
Studies demonstrate up to a ~40% success rate in converting patients back into normal sinus rhythm.
Benefits of vagal maneuvers:
Safe for most patients*
Avoids use of adenosine, a medication that is associated with side effects like lightheadedness, chest discomfort, vomiting, and severe anxiety, all of which can be very concerning to patients.
*see contraindications to specific vagal maneuvers below
Brief Physiology of Vagal Maneuvers:
https://www.hopkinsmedicine.org/health/conditions-and-diseases/anatomy-and-function-of-the-hearts-electrical-system
Normal sinus rhythm starts with an electrical impulse at the sinoatrial (SA) node → atrial tissue → atrial contraction → AV node → His-Purkinje system → ventricular myocardium → ventricular contraction
https://www.cprseattle.com/blog/slow-down-youre-going-too-fast-svt-and-the-modified-valsalva-maneuver
SVT (specifically AVRT/AVNRT) is most commonly caused by a re-entry conduction pattern involving a retrograde accessory pathway from the ventricles to the atrium, bypassing the SA node.
Vagal maneuvers work by stimulating the vagus nerve, which slows the impulse at the sinus node, conduction at the AV node, and lengthens the AV node refractory period.
Initially, pressure against a closed glottis results in increased intrathoracic pressure → increase in blood pressure → increased aortic pressure → baroreceptor activation → increased parasympathetic output to the heart via the vagus nerve → decreased heart rate.
Ghazal, S.N. Valsalva maneuver in echocardiography. J Echocardiogr 15, 1–5 (2017).
During the straining period of the vagal maneuver, there is a prolonged period of increased intrathoracic pressure → decreased venous return → decreased cardiac output → reflexive increase in HR to maintain stroke volume.
When the maneuver is stopped, there is sudden decrease in intrathoracic pressure → increased venous return and right atrial pressure → increased blood pressure and aortic pressure → reflexive decrease in heart rate and termination of SVT
Types of Vagal Maneuvers:
http://healthcaresciencesocw.wayne.edu/cnm/8_2.htm
The Valsalva Maneuver
Main take away: creating pressure against a closed glottis
Success rate: 5 – 20%
Contraindications:
Unstable SVT
SVT due to acute MI
Aortic Stenosis
Carotid artery stenosis
Glaucoma or retinopathy
https://www.medicalnewstoday.com/articles/322661
Methods:
Gag
Cough
Have patient plug nose, close mouth, and try to blow air out for 15 seconds
Blow on a 10mL syringe for 15 seconds
Bear down and strain by trying to push the air out of the lungs while closing nose and mouth. Attempt for 15 seconds
with 45 seconds of passive leg raise
https://www.ecgmedicaltraining.com/wp-content/uploads/2016/06/REVERT-Trial-SVT.jpg
The Modified Valsalva Maneuver (REVERT Trial)
Main take away: Valsalva using 10mL syringe + passive leg raise to improve venous return
Success Rate: In the RCT REVERT, the modified valsalva maneuver demonstrated 43% success rate, significantly more than valsalva maneuver alone (only 17%).
Contraindications: same as the valsalva maneuver
Methodology:
Place patient in a sitting position
Have patient blow into a 10mL empty syringe for 15 seconds (~40mmHg)
After 15 seconds, immediately recline patient into supine position with 45 seconds of passive leg raise
https://www.grepmed.com/images/10366/algorithm-tachycardia-treatment-management-peds
Ice Water on the Face
Main take away: In pediatric patients who cannot follow directions, placing a bag of ice water over their forehead and eyes is the first line vagal maneuver. This stimulates the vagus nerve via activating a “diving reflex”, causing the child to valsalva.
Success rate: 33-63%
Contraindications:
Unstable SVT
Methodology: Place a bag of iced water over an infant's eyes and forehead and hold for 15-30 seconds. Do not cover the infant's nose or mouth
https://coreem.net/core/avnrt/
Carotid Massage
Main take away: Stimulates the carotid sinus, which stimulates vagus nerve, activating parasympathetic response and slows impulse at SA node. Generally, it has fallen out of favor given the risk of precipitating stroke in patients with carotid stenosis.
Contraindications:
Unstable SVT
Carotid bruit
Prior TIA or CVA in past 3 months
Pediatric patients
Methodology: Patient in a supine position with the neck extended, and applying pressure to one carotid sinus for approximately 10 seconds
References:
1. Appelboam A, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomized controlled trial. The Lancet 2015; 386 (10005): 1747-1753.
2. Ghazal, S.N. Valsalva maneuver in echocardiography. J Echocardiogr 15, 1–5 (2017). https://doi-org.turing.library.northwestern.edu/10.1007/s12574-016-0310-8
3. Manole MD, Saladino RA. Emergency department management of the pediatric patient with supraventricular tachycardia. Pediatr Emerg Care. 2007 Mar;23(3):176-85; quiz 186-9. doi: 10.1097/PEC.0b013e318032904c. PMID: 17413437.
4. Niehues LJ, Klovenski V. Vagal Maneuver. [Updated 2021 Jul 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551575/
5. Patti L, Ashurst JV. Supraventricular Tachycardia. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441972/
6. Salim Rezaie, "The REVERT Trial: A Modified Valsalva Maneuver to Convert SVT", REBEL EM blog, September 14, 2015. Available at: https://rebelem.com/the-revert-trial-a-modified-valsalva-maneuver-to-convert-svt/.
Expert Commentary
Thank you for this excellent review of the non-pharmacologic options for managing SVT in the ED. At one point or another in my career, I have tried them all…. and I think one of the most important things to remember about these options is: there are very few harms that can result from giving them a try.
Although the individual success rate of each maneuver is not high, there is not a lot to be lost in attempting one (or more) of these techniques while other activities are in-motion to start pharmacologic therapy should the non-pharmacologic maneuvers fail. I typically do not delay having nursing establish an IV and pulling medications in preparation for pharmacologic management given that the maximal reported success rate is 43%; however, assuming no contra-indications, it doesn’t hurt try. Even in the most highly functioning EDs, it takes a few minutes to get a patient on a monitor, get continuous EKG set up and get pharmacy / nursing colleagues to bedside for administration of adenosine (or other meds) with real-time EKG tracing. It is during those minutes that I make use of these maneuvers to see if the pharmacologic therapy can be avoided.
Pre-2015, I could count on one hand the number of times I’d been successful with a vagal maneuver; however, since publication of the REVERT Trial, I have personally found using Modified Valsalva Maneuver to be more successful than Valsalva alone and have been able to avoid adenosine for numerous patients. Consider reviewing the prior NUEM blog post that discusses the REVERT Trial results in detail.
Since starting to personally use this Modified Valsalva technique in ~2016, I have adopted a few practices that may be helpful. First, I explain to the patient that we are going to ask them to do some stuff that may seem silly, but it might help them to avoid medications and I caution them that it only works ~40% of the time. Second, I’ve taken to holding up my phone with the digital timer facing the patient so they can see the seconds counting down. I’ve subjectively found that it helps them to “hang in there” and maintain the breath hold longer than without looking at a timer. Without a timer, we (doctors/nurses) tend to unintentionally “speed-up” our pace of counting as we see the patient fatiguing and therefore don’t achieve a full 15 second count. Similarly, I advocate for using your phone or a wall-clock to maintain the leg raise for a full 45 seconds. This adherence to the time intervals ensures that you’re sticking to the true technique of the maneuver rather than approximating the technique and potentially diminishing its effect. Third, if it works, I review the steps with them again and send them home with an empty syringe (and they think you’re a magician). If it fails, you already counseled them that it would likely fail; you’ve lost neither time nor trust.
Finally, I have noticed that successful or not, having a few doctors and nurses cheer a patient on to maintain the breath hold builds a spirit of trust and camaraderie. This trust is hopefully helpful to the patient…particularly when we start to explain how we are going to give a medicine that will temporarily stop their heart and make them feel transiently terrible.
In conclusion, give it a try. If these maneuvers fail, then move on. In the stable patient, consider adenosine or calcium channel blockers (see NUEM blog post on CCB as an alternative to adenosine in SVT here).
Danielle M McCarthy, MD
Vice Chair for Research, Department of Emergency Medicine
Associate Professor, Emergency Medicine
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Kilbane, K, Leibowitz, M (2024, Jul 14). Vagal Maneuvers Simplified. [NUEM Blog. Expert Commentary by McCarthy, M]. Retrieved from http://www.nuemblog.com/blog/vagal-maneuvers-simplified