Written by: Ashley Segobiano, MD (NUEM ’28) Edited by: Keara Kilbane, MD (NUEM ’25)
Expert Commentary by: David Haidar, MD
Welcome to the NUEM SonoPro Tips and Tricks Series where Local and National Sono Experts team up to take you scanning from good to great for a particular diagnosis or procedure.
For those new to the probe, we recommend first reviewing the basics in the incredible FOAMed Introduction to Bedside Ultrasound Book, 5 Minute Sono, and POCUS Atlas. Once you’ve got the basics beat, then read on to learn how to start scanning like a Pro!
Did you know?
Pericardial effusions have many different etiologies with the most common causes being malignancy, idiopathic, infectious/inflammatory, iatrogenic, metabolic, and bleeding/anticoagulation (1).
Mortality up to 100% depending on etiology of pericardial effusion with survival directly associated with time to diagnosis and intervention (1).
The presence or even size of a pericardial effusion does not inherently lead to tamponade physiology, rather it is the rate at which the pericardial effusion accumulates and the compliance of the pericardium that leads to infringement upon the dynamics of the heart and ultimately hemodynamic instability (3).
Point of care echocardiography performed by Emergency Medicine Physicians was able to detect pericardial effusion with a sensitivity of 96%, specificity of 98%, and overall accuracy of 97.5% (2).
SonoPro Tips- How to Scan like a Pro
Four POCUS Findings of Pericardial Tamponade (4):
The below sonographic images exhibit the aforementioned findings listed from LEAST specific to MOST specific for cardiac tamponade:
Plethoric Inferior Vena Cava
In tamponade physiology, the IVC is considered to be plethoric when it is measured to be greater than 2cm.
With patient inhalation, you will see minimal to no IVC collapse, indicating hindrance in venous return.
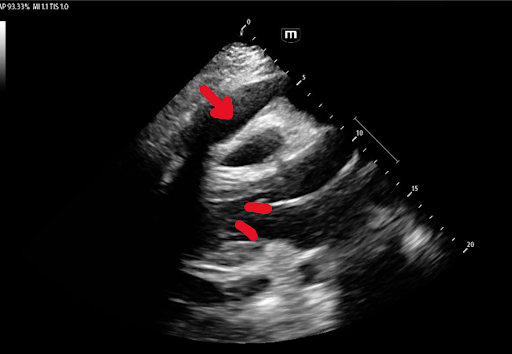
Right Atrial Systolic Collapse
The best view to see right atrial systolic collapse is the apical 4-view. If you are unable to properly visualize the right atria with the apical 4-view, try the subxiphoid approach!
Systole is defined when the mitral valve is closed. Notice the fragile wall of the right atrium collapsing during systole. This is an early and very concerning sign of pericardial tamponade.
Right Ventricular Diastolic Collapse
You can identify right ventricular diastolic collapse in all 4 cardiac windows, however we suggest starting with the parasternal long and short views to exhibit this finding in at least two views.
Diastole is defined when the mitral valve is open. During right ventricular diastolic collapse, you will appreciate that when the mitral valve is open that the fragile right ventricular wall collapses inward toward the interventricular septum. If you are seeing an associated pericardial effusion, this is highly concerning for tamponade physiology.
Another way to identify RV diastolic collapse is to use M-Mode in the parasternal long view. Place the M-Mode tracing through the RV and mitral valve and run the tracing. When the mitral valve is open (diastole), you can see the RV collapsing on the tracing.
Mitral/Tricuspid Valve Inflow Variation
Remember the classic teaching that pulsus paradoxus may be present in cardiac tamponade? Mitral valve inflow variation is considered the pulsus paradoxus of ultrasound!
The best way to calculate mitral and tricuspid valve inflow variation is to obtain an apical 4 view.
To calculate mitral valve inflow variation, place the ultrasound on pulse-wave doppler mode with the focus in the left ventricle just beyond the mitral valve, where the valve leaflets touch. Then identify the E wave (labeled above), which represents early diastolic filling of the left ventricle, and measure the difference between the E wave during inspiration and expiration. A difference of > 25% in the setting of pericardial effusion is concerning for tamponade physiology.
Repeat the same steps to calculate tricuspid valve inflow variation, but place the doppler indicator in the right ventricle, just beyond the tricuspid valve. A difference of >40% is concerning for tamponade physiology.
What to do next:
If otherwise not clinically contraindicated, proceed with pericardiocentesis (5)!
Consider administering small bolus fluid to optimize preload and epinephrine drip to avoid bradycardia and myocardial depression (3).
Position the patient for optimal oxygenation as intubation should be avoided at all costs due to the pressure dynamics that can result and potential worsening of tamponade physiology (3).
Using your newly honed ultrasound capabilities, locate the largest, shallowest fluid pocket clear of vital structures and numb locally for patient comfort (1).
Utilize ultrasound to guide your needle and to confirm catheter placement (1).
Pericardial fluid should be aspirated to assess for hemorrhage and then slowly drained to avoid pericardial decompression syndrome (1).
Consult cardiology for ICU admission and further management.
Where to Learn More (Hyperlinked References):
Expert Commentary
Thank you Dr. Segobiano and Dr. Kilbane for this great review of sonographic evidence of tamponade physiology! This is a great example of how bedside ultrasound can be rapidly used for life saving diagnoses. Ultrasound is just a single data point in the overall assessment of your patient and no single view is going to give you the diagnosis, but concerning sonographic findings in a patient who looks unwell will definitely help in making your diagnosis of tamponade!
When scanning it can be hard to tell when exactly the RA or RV are collapsing. I recommend saving clips and then reviewing the videos after you’re done scanning. You can pause a video and scroll through the images until you see when the mitral valve is open (diastole) and when it’s closed (systole). At this point you can compare the sizes of the chambers to get a better idea of the presence or absence of collapse.
Mitral valve inflow variation will be your most specific finding, and technically the most challenging to obtain. If you’re struggling to obtain the views above, you can have patients lift their left arm over their head and lay left lateral decubitus to help bring the heart closer to the chest wall and improve your images.
This sonographic surrogate for pulsus paradoxus occurs due to ventricular interdependence - which is when changes in one ventricle’s pressure affects the pressure in the other ventricle. This occurs naturally during inspiration and expiration, and is exaggerated when there is pressure in your pericardium from fluid - the RV can’t expand due to fluid in the pericardium so it pushes on the septum and in turn your LV, decreasing LV filling and affecting your cardiac output. This phenomenon is what leads to pulsus paradoxus and can be measured by looking at the changes in MVIV through the respiratory cycle.
When measuring MVIV, make sure you are comparing E-wave to E-wave. Accidentally comparing an E-wave to an A-wave will give you a falsely elevated difference in MVIV.
Once you’ve made the diagnosis, if you have to emergently perform a pericardiocentesis at the bedside remember, go where the fluid pocket is biggest, and make sure to perform this under ultrasound guidance!
David Haidar, MD
Clinical Assistant Professor
Feinberg School of Medicine
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Segobiano, A., Kilbane, K. (2025, Oct 17). Sono Pro Tips and Tricks for Promptly Identifying Cardiac Tamponade. [NUEM Blog. Expert Commentary by Haidar, D]. Retrieved from http://www.nuemblog.com/blog/sonopro-tips-and-tricks-for-tamponade