Anticoagulation in Distal DVT
Written by: William LaPlant, MD (NUEM PGY-3) Edited by: William Ford, MD (NUEM PGY-4) Expert commentary by: Kelsea Caruso, PharmD
Currently there is significant heterogeneity in the treatment of distal deep vein thromboses (DDVTs), which are DVTs that occur distal to the popliteal fossa. What is the best course of action when a reasonably healthy patient has a new calf DVT?
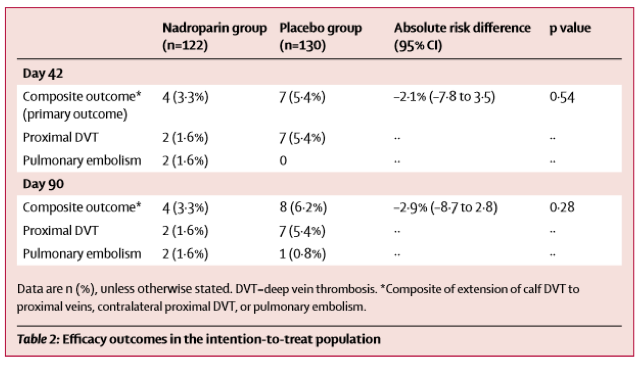
The CACTUS trial was a randomized, placebo-controlled, double-blinded trial prospectively assessing anticoagulation for calf DVTs [1]. Notably, the trial was met with slow enrollment resulting in termination of the study prior to enrollment of the prespecified sample size, meaning that it was underpowered to detect a significant difference between the groups. It only enrolled about half of the participants it had intended to, with an initial 90% power to detect a 70% risk reduction in the composite outcome: development of a proximal DVT or symptomatic PE by day 42. This power study assumed a 10% incidence of the primary outcome in the placebo group.
As you can see, in both groups the progression to proximal DVT or PE was quite low. As there were only 12 total composite events (DVT extension, PE), making a comparison between groups with any degree of certainty impossible. This study met neither their enrollment goals (only enrolling half the participants) nor the predicted incidence of the composite outcome (half the projected amount), so it was quite significantly underpowered to detect a difference.
Notably, the study also did not enroll pregnant women, patients with a previous DVT, recent PE, or recent malignancy. These patients were likely not enrolled due to their higher risk of progression, which may have biased the results towards treatment. As such, the results of this trial could never be applied to these groups.
Unfortunately, given the slow recruitment in the CACTUS trial as well as the low event rate of the composite outcome, the likelihood that this will be studied again in a prospective, double-blinded manner is unlikely. As such, we will need to put the CACTUS trial into context of retrospective evidence to try to identify an ideal practice pattern.
With regard to the retrospective data available:
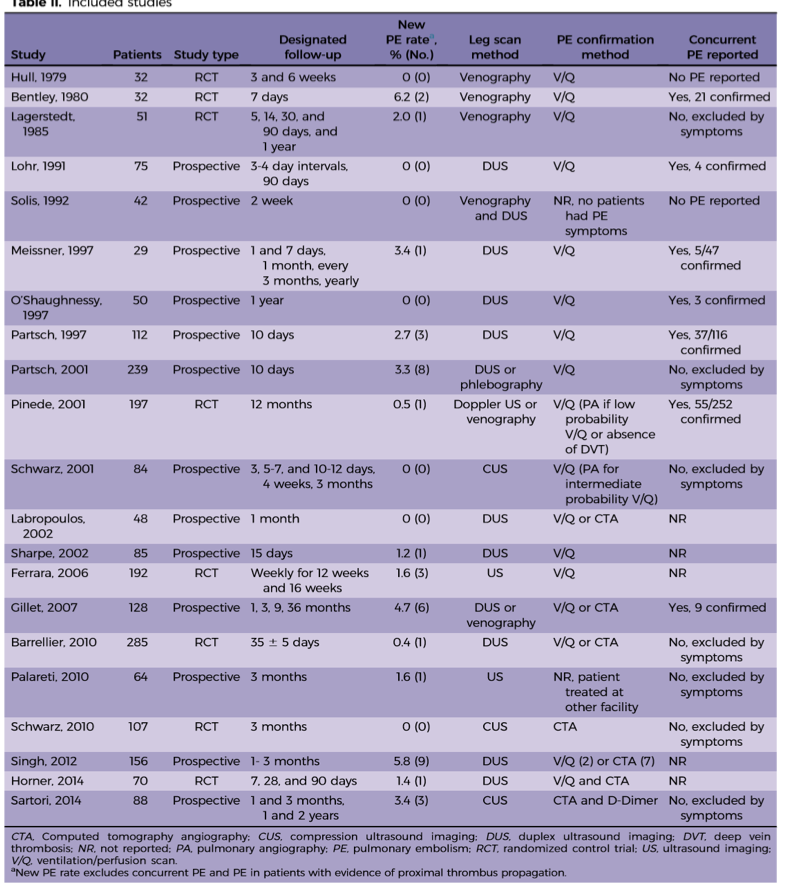
In a 2016 metanalysis, the incidence of PE from DDVT was 0% to 6.2% [median 1.1%] [2], which is in line with the results from the CACTUS trail. As you can see in the chart below, there is some heterogeneity to the results, likely due to the wide variety in study methodology.
Based on the above evidence, what are the best management options? A recent review article (which includes data from CACTUS) offers two suggestions [3]:
The most conservative management will still be anticoagulation of the isolated DDVT. This should be standard for patients with cancer or other pro-thrombotic state that would place the patient at high risk for the development of DVT.
Deferred anticoagulation with follow up ultrasound can be used for patients without significant thrombotic risk factors. You can engage in shared decision making and discuss the risks for bleeding in your patient against the 4-5% risk for clot progression and 1% risk for PE (based on the CACTUS trail as well as retrospective data).
If you decide against anticoagulation in the emergency department, follow up imaging would be recommended in 1-2 weeks to evaluate for progression. This tight follow up window would help to ensure clot progression is identified early and would allow the patient to readdress anticoagulation with his/her primary care physician.
Expert Commentary
Thank you for this really great summary! I think you are bringing up a dilemma that we see quite often in the Emergency Department and one that, unfortunately, still doesn’t have much data to help guide our treatment recommendations. The CHEST guidelines for VTE disease were most recently updated in 2016 and do not include the results of the CACTUS trial or the results of the mentioned meta-analysis. Their recommendation is to treat an unprovoked DVT (distal or proximal) with anticoagulation for at least 3 months.
The CACTUS trial questioned if this is required for all patients, primarily focusing on those with an isolated calf DVT. The CACTUS trial had some interesting results, but, like you mentioned, a huge patient population was excluded.. We can only extrapolate this data to a very small group of people: young (average age ~50 years old in the trial), healthy and without any risk factors for VTE. Also, the study drug utilized in the trial was nadroparin, a low molecular weight heparin, which is not available in the US. It would have been more applicable to clinical practice if this trial had utilized a direct-oral anticoagulant like rivaroxaban or apixaban. If these were used the safety results could have potentially been reduced.
So the question remains… to anticoagulate or not to anticoagulate? Here are my final thoughts:
The patients you can think about deferring anticoagulation are those without any VTE risk factors (cancer, obesity, immobility, those on estrogen therapy etc.).
As mentioned, this should be a discussion with the patient so they understand the risk of deferring anticoagulation. They should have adequate follow-up and understand the signs and symptoms of a pulmonary embolism.
The patients that should be anticoagulated are those that have any risk factor for VTE or patients from the previous point that choose treatment.
The anticoagulant should be selected by keeping patient specific factors in mind like past medical history, renal function and current medications
Unlike the CACTUS trial, try and prescribe oral therapy. Your patients will thank you if they don’t have to inject themselves daily.
Kelsea Caruso, PharmD
Emergency Medicine Clinical Pharmacist
Northwestern Memorial Hospital
How To Cite This Post
[Peer-Reviewed, Web Publication] LaPlant W, Ford W. (2019, May 6). Anticoagulation in distal DVT. [NUEM Blog. Expert Commentary by Caruso K]. Retrieved from http://www.nuemblog.com/blog/distal-dvt
Other Posts You May Enjoy
Resources
Righini M, Galanaud J, Guenneguez H, et al. Anticoagulant therapy for symptomatic calf deep vein thrombosis ( CACTUS ): a randomised , double-blind , placebo-controlled trial. 2017;3(December 2016). doi:10.1016/S2352-3026(16)30131-4.
Wu AR, Garry J, Labropoulos N, Brook S. Incidence of pulmonary embolism in patients with isolated calf deep vein thrombosis. J Vasc Surg. 2016;5(2):274-279. doi:10.1016/j.jvsv.2016.09.005.
Robert-ebadi H, Righini M. Management of distal deep vein thrombosis ☆. Thromb Res. 2017;149:48-55. doi:10.1016/j.thromres.2016.11.009.