Author: Hashim Zaidi, MD (EM Resident Physician, PGY-1, NUEM) // Edited by: Andrew Ketterer, MD (EM Resident Physician, PGY-3, NUEM) // Expert Reviewer: Scott Dresden, MD
Citation: [Peer-Reviewed, Web Publication] Zaidi H, Ketterer A (2016, April 19). The New And Improved Valsalva: The Revert Trial. [NUEM Blog. Expert Peer Review by Dresden S]. Retrieved from http://www.nuemblog.com/blog/the-new-valsalva
Introduction
It’s a busy day in the emergency department and before you know it someone is being wheeled back from triage with a heart rate of over 200. Yikes! You put on your cardiology hat and take a look at the EKG right away as the patient is being roomed.
You adeptly recognize this to be supraventricular tachycardia (SVT), most likely AV or AV nodal reentrant tachycardia given its regular and narrow QRS complex (but you also consider atrial tachycardia!). Your patient is a 29 year old female with a known history of SVT and has been cardioverted in your department before. She is hemodynamically stable, awake, alert, and following commands without difficulty in between tweeting about her medical experience.
With over half a million individuals with known paroxysmal SVT living in the US and almost 89,000 new cases diagnosed each year, these patients are bound to show up in the ED when they are unable to self-terminate their arrhythmias [3]. Patients with lone SVT without other cardiovascular disease are most often young females of childbearing age.
As you ponder the prevalence of SVT your nurse brings you back to reality and asks you for your next move on this patient. After obtaining access, attaching them to multiple monitors, and making sure the crash cart is handy, you mention you would like to try some vagal maneuvers, in particular your favorite: the Valsalva maneuver. This is received with audible groans from all parties involved, from your colleagues to the patient. They cite these maneuvers as having a cardioversion success rate as low as 5%, and are rarely as dramatic or exciting as the push of adenosine [4].
The ECG of Supraventricular Tachycardia
Old Valsalva rolling in his grave at the idea of changing his maneuver
What if there were a way to improve the Valsalva maneuver? After all, its noninvasiveness and lack of appreciable side effects (in most populations) make it a reasonable thing to try first, if only it ever worked. Appelboam and his colleagues thought the same and reported on a modified version of the Valsalva they felt was more successful for a patient who could not tolerate electrical cardioversion [5]. This maneuver involved a traditional Valsalva to 40 mmHg for 15 seconds, followed by lying supine with a passive leg raise to 45 degrees for another 15 seconds before returning to sitting upright. Now I know what you’re thinking: that’s all fine and dandy for one patient across the pond, but does a modified Valsalva actually cardiovert more patients presenting to the ED in SVT compared to the traditional Valsalva maneuver? With that question in mind Appelboam et al. performed a randomized control trial to investigate.
The Study
The REVERT trial published in The Lancet this past August described a randomized multicenter parallel group trial that gave its two study groups instructions to complete either the traditional Valsalva maneuver or the modified maneuver. Eligible patients were adults over 18 years of age who presented in stable SVT to ten emergency departments in England. All patients had a screening 12-lead EKG prior to any treatment and only those with regular, narrow-complex tachycardia (QRS less than 120msec) were included. Patients in suspected atrial fibrillation or atrial flutter were excluded, as were those who had any indications for immediate cardioversion (discretion left to providers) or a systolic pressure less than 90 mmHg. Additionally, if the patients were unable to perform Valsalva or its modifications (e.g. pregnant patients in the 3rd trimester, patients who were unable to lie flat, or patients with spinal stenosis, aortic stenosis, recent MI, any reason to feel discomfort from the maneuver, etc.) they were also excluded from this trial. While investigators were blinded during analysis, providers could not be for obvious reasons: once the patients were randomly assigned to a treatment arm via envelope the providers were unmasked to the group assigned for treatment purposes.
Once randomized to a treatment arm, patients performed either a more common sitting Valsalva(termed “stay sitting Valsalva") or the modified version as reported by Appelboam et al. Both group started procedures similarly with 15 seconds of semi-recumbent (45 degrees) Valsalva to a pressure target of 40 mmHg as measured by an aneroid manometer with the goal clearly marked for patients and providers. The “stay sitting” group then remained in the same position for the next 60 seconds before reassessment of the cardiac rhythm by 3-lead ECG. Following their 15-second Valsalva maneuver, patients in the modified group were laid supine (0 degrees) with their legs raised by staff members to 45 degrees for 15 seconds, and were then returned to semi-recumbent for 45 seconds before rhythm analysis. If sinus rhythm was not restored a second attempt in the same allocated manner was made; further treatment was left to the discretion of the clinician. 12-lead ECGs were obtained at one minute following each attempt to assess rhythm.
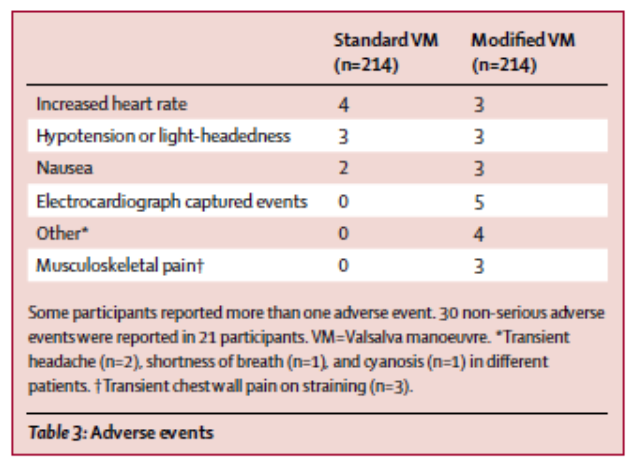
Overall the study showed significantly higher rates of sinus rhythm achieved at one minute in the modified Valsalva group as compared to the traditional group (Table 2). 43% of the modified group achieved sinus rhythm at one minute compared to 17% of the traditional group with an odds ratio of 3.7 (95% CI 2.3-5.8). Use of adenosine was lower in the modified group (69% vs 50%, P<.0002) and a significantly greater number of the traditional group required any emergency anti-arrhythmic treatment (80% vs 57%, P<.0001). Length of stay in the ED and admission rates were equivalent in both groups. No serious adverse events were reported in either group, and although the modified group had higher absolute numbers of non-serious adverse events, this did not represent a statistically significant difference (Table 3). None of the adverse events required additional treatment and all were reported to be self-limiting.
Analysis
This study is a well conducted, well organized randomized control trial studying a simple and (from this one study) effective strategy to improve vagal cardioversion for patients presenting in narrow regular SVT. Studies like these often remind clinical researchers that more complex is not always better. The major strength of this study is its simplicity: a two-arm randomized study with one dependent variable is clinical science in its purest form. The investigators here had a hypothesis that this modified maneuver had some greater clinical effectiveness and did an effective job researching it. The study was powered effectively (for a 12% difference), randomized appropriately, and conducted good retrospective reviews on 12 leads to confirm rhythms. One caveat the authors mention is that clinicians were not masked to allocation but since the control Valsalva was termed “sitting up Valsalva” ; this is a common method of vagal maneuver and may be identified as the control arm. Most ED physicians would be able to recognize a traditional Valsalva and would also recognize deviations from the standard vagal maneuver. This may have led to more consistent or appreciated efforts in the treatment arm compared to the control. The authors also acknowledge they had higher rates of protocol violations in the form of ineligible rhythms but this was nearly equivalent in both arms. While the maneuver itself is simple and practically very feasible, the authors also used a labeled standardized manometer to achieve desired pressures. One solution is to have the patient blow into a 10cc syringe: the authors note that if enough pressure is produced to move the plunger, a nearly equivalent amount of pressure is generated [7]. This by itself has significant implications in instructing patients to perform the Valsalva maneuver prior to visiting the ED, potentially saving resources in the prehospital and hospital realms, and raises the already well defined external validity of the study. Further studies need to be conducted independently and in other populations to confirm this study's results.. Additionally, studies evaluating the use of this modified maneuver in the prehospital setting, comparisons with other Valsalva variations, and studies with fewer protocol violations would all help to characterize the modified Valsalva’s utility.
The new and improved Valsalva
One barrier to vagal maneuver efficacy in SVT may the the variation in style and procedure in which practitioners use it. By having a standardized protocol with some proven efficacy such as in this study, practitioners may perform more consistent, dedicated efforts for vagal cardioversion prior to reaching for electricity or pharmacology. This study demonstrates that a modified Valsalva is effective in converting nearly half of all patients with narrow, regular SVT, meaning that only three patients would need to be treated to prevent one from undergoing more invasive means of cardioversion. While the need for admission or time spent in the ED were unchanged in this study, this appears to be a cost-effective, simple strategy that could potentially decrease the need for pharmacologic cardioversion in and out of the hospital.
Expert Review
This is a great summary of REVERT, a simple yet elegant study. I can sympathize with the resident in the case summary who is excited to use a Valsalva maneuver, and save the patient the sensation of having her heart stopping, only to have a group of well-seasoned emergency nurses, techs, and attendings, groan at his or her naiveté. In fact, when I first reviewed this study, my first response was, “Valsalva? That never works!” But after reading the article, I realized, not only was I spelling Valsalva manoeuvre wrong, I was doing it wrong too. For a video example on how to do a modified Valsalva manoeuvre correctly, readers should be sure to watch the Lancet video embedded in the post. The keys are the “ready, steady, blow” command followed by blowing into a 10cc syringe enough to move the plunger, and then lying the patient flat whilst elevating his or her legs.
This study is beautiful for many reasons:
Internal validity: RANDOMIZED CONTROLLED TRIAL – the gold standard, obviously tough to blind patient to the intervention, but otherwise, you couldn’t ask for more. They had good distribution of baseline characteristics as seen in table 1 of the study– with even perhaps a slightly sicker population in the treatment group (slightly more patients with previous ablation, ischemic heart disease, diabetes, and hypertension)
External validity: MULTI-CENTERED ED trial – again, can’t ask for much more than that, perhaps someone might suggest we repeat it in the US, so they can boost their publication record, but I can’t see any reason why it wouldn’t work on this side of the pond as well as it does over there. Also their exclusion criteria were few, allowing for more generalizability – we love this in the ED. They excluded “unstable patients with SBP <90 or an indication for immediate cardioversion, and those in atrial fibrillation or flutter. Additional exclusion criteria were: aortic stenosis, recent myocardial infarction (it is not clear how recent is recent), glaucoma or retinopathy, inability to lie flat, or have legs lifted, they were not included in this study.
Cost to implement: $0.66 for a 10cc syringe on Amazon (probably cheaper than for the hospital)
Limitations of this study:
The study was not powered to measure adverse events.
The importance of the outcomes is not clear. Though they met their primary objective of increasing sinus rhythm at 1 minute after vagal manoeuvre, and decreased the amount of anti-arrhythmic drugs (adenosine and others), it isn’t clear how important that is to patients. Patient may just want you to get their heart to stop racing, they don’t care how you do it.
There was no improvement in operational outcomes: discharge home from the ED, ED length of stay
Overall, I think of this study as a great example of emergency medicine research. It is a simple, well executed study with solid methods. Clinically I see using modified Valsalva as a no risk, low reward scenario. I plan to use it in the future, and will likely prevent 1 in 3 patients from being hooked up to continuous 12 lead while the whole ED stands around watching a nurse slam adenosine through an 18 gauge IV, and then waiting for the patient’s heart to stop and then restart again. I won’t pretend it’s going to help us with our ED throughput though.
How to incorporate this study into practice:
Look at the patient’s vital signs, SBP <90 ? Think synchronized cardioversion (50-100 J)
Ask if they have aortic stenosis, a recent MI, glaucoma, or retinopathy
Tell them what you plan to do, if they say, “I can’t lie down,” or "Look at my gravid abdomen", or "I don’t think I can let you lift my legs like that", then think about adenosine (6, 12, 12 mg)
Give them a syringe, say, “Ready, steady, blow, 4, 3, 2, 1” (as they blow on the syringe), lie them down, tip their legs up and watch their HR slow down
If it works, perhaps teach them how to do this themselves if it happens again outside the hospital
If it doesn’t work, grab the drugs, but hey, at least you tried
Scott M. Dresden, MD, MS, FACEP
Assistant Professor; Northwestern University; Department of Emergency Medicine; Center for Healthcare Studies
References
Image Credit: Google Image terms “Cardiology Hat” <http://rlv.zcache.com/i_love_cardiology_hat r41accbe172c84aebba0c4174f7cfc0af_v9wqr_8byvr_324.jpg>
Image Credit: Life in The Fast Lane. Accessed October 11th 2015. <http://lifeinthefastlane.com/ecg-library/svt/>
Orejarena LA, Vidaillet H, Destefano F, et al. Paroxysmal supraventricular tachycardia in the general population. J Am Coll Cardiol. 1998;31(1):150-7.
Taylor DM, Wong LF. Incorrect instruction in the use of the Valsalva manoeuvre for paroxysmal supraventricular tachycardia is common. Emerg Med Australas 2004; 16: 284–87.
Appelboam A, Gagg J, Reuben A. Modified Valsalva manoeuvre to treat recurrent supraventricular tachycardia: description of the technique and its successful use in a patient with a previous near fatal complication of DC cardioversion. BMJ Case Rep. 2014;2014
Image Credit: Google Image Antonio Valsalva Accessed October 11th 2015 <http://goflightmedicine.com/wp-content/uploads/2014/05/Antonio-Valsalva.jpg>
Smith G, Boyle M. The 10ml syringe is useful in generating the recommended standard of 40mmHg intrathoracic pressure for the Valsalva manoeuvre. Emerg Med Aust 2009; 21: 449–54.