Written by: Justine Ko, MD (NUEM PGY-3) Edited by: Terese Whipple, MD (NUEM PGY-4) Expert commentary by: Matt Levine, MD
Pelvic Ring Fractures
Overview
Pelvic ring fractures make up about 3% of skeletal fractures [1]. In the emergency department, they are often seen with high-impact blunt trauma, such as MVCs, crush injuries, or falls.
The pelvis consists of the sacrum and the two innominate bones, which are made up of the ilium, ischium, and pubis [2]. The sacrum and the innominate bones together form a posterior arch and an anterior arch that join to make a ring, also known as the pelvic inlet. The stability of the pelvis is enforced by ligaments: the sacroiliac ligaments, the sacrospinous ligaments, and sacrotuberous ligaments [2]. The ligaments and bones together give the pelvis vertical and rotational stability.
Pelvic ring fractures carry a significant mortality, ranging from 15-25% in closed fractures, and as much as 50% in open fractures [3]. They are often associated with other high-mortality injuries as well, such as chest injuries, spinal injuries.
What are the mechanisms associated with these injuries?
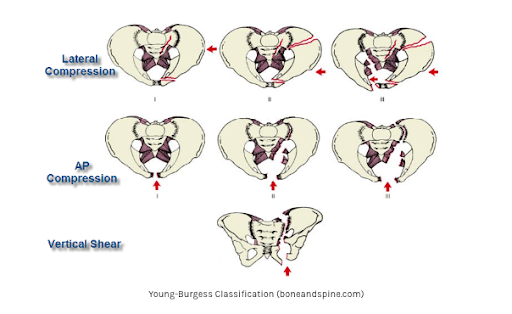
The Young-Burgess classification system categorizes injury patterns based on the mechanism of injury and the forces applied: anteroposterior compression (APC), lateral compression (LC), and vertical shear (VS) [1]. The most common mechanism is lateral compression, which occurs when lateral forces are applied to the pelvis (as the name would suggest). APC injuries result in the classic “open book” pelvic fractures (Figure 1).
Figure 1
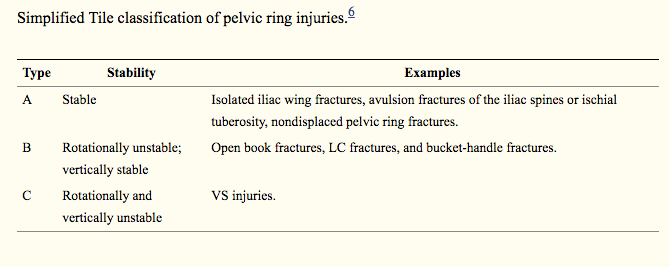
Figure 2
Anteroposterior compression: causes disruption of the pubic symphysis. A normal pubic symphysis should not exceed 5mm. Injuries where the symphysis widening is <2.5cm, with no significant posterior column injury or other fractures, are usually considered stable. APC injuries are often associated with significant blood loss, as the pelvic volume increases and can store more blood [4].
Lateral Compression: considered rotationally unstable. This mechanism causes the pelvic volume to decrease, and therefore, is associated with less blood loss [4].
Vertical shear: the most unstable, often associated with axial loading of the hemipelvis, such as with a fall or a jump from a height.
What exam findings should I look for?
During a trauma workup, visual inspection for leg-length discrepancy or rotation of the pelvis may provide clues to a hip or pelvic injury. You may assess for stability of the pelvis by applying downward and medial pressure to the bilateral iliac crests. Apply pressure gently and slowly to avoid disruption of any possible clots that may have formed.
A digital rectal exam should also be performed to assess for spinal cord injury and frank blood. In males, the meatus should be assessed for possible bladder or urethral injury.
X-ray reading tips
Check the 3 circles! (Figure 3)
Pubic inlet
Two obturator foramina
Check for irregularities along the circles
In general, a vertical fracture pattern will be associated with APC or VS mechanisms. Horizontal fracture patterns will be associated with LC. [7]
Figure 3
Check the lines!
ilioischial line (orange line in Figure 4)- disruption suggest posterior column fracture [5]. The posterior column involves the posterior half of the acetabulum and extends to the ischial tuberosity [4].
iliopectineal line (red line in Figure 4)- disruption suggests anterior column fracture [5]. The anterior column involves the anterior half of the acetabulum and extends to the lateral half of the superior pubic ramus [4].
It’s a circle! If it breaks in one location, it likely broke in another place. Be wary of isolated rami fractures in the setting of high-impact trauma!
Figure 4
Management
As always, still stick to your ABCs!
Initiate blood transfusion early for patients in shock
Hemodynamic instability occurs in about 10% of these injuries [1]
Try to obtain IV access above the pelvis if a pelvic fracture is suspected.
Stabilize the pelvis with a TPOD or a sheet for patients with open book pelvic fractures
Apply over the GREATER TROCHANTERS
Do not apply a compressive device for isolated lateral compression pelvic fractures as the device can cause further compression and worsen the displacement [4].
If the hemorrhage or hypotension is suspected to be from pelvic hemorrhage, activate IR early.
If stable, obtain a CTA of the pelvis to assess for vascular injury
What other injuries should I look for?
Urologic Injury: incidence in pelvic fractures is ~5%. Patient with blood at the meatus will need a retrograde urethrogram and then a cystogram [4].
Neurologic Injury: pelvic fractures can be associated with plexus injuries and even cauda equina syndrome. Check for rectal tone and saddle anesthesia [4].
Gynecologic injury: blood a the introitus can represent urethral injury or an open pelvic fracture [4].
Expert Commentary
Dr Ko has provided a high yield concise guide of the key cognitive and clinical features of pelvic fractures. A few points worthy of further emphasis:
When examining for pelvic instability, do not rock on the pelvis to further open it. Instead, compress medially to feel instability while closing, rather than opening, the pelvis.
For most studies we order, we have the luxury of waiting for a formal report. Pelvis x rays are one of the few radiographic studies that the Emergency Physician must be able to rapidly interpret independently at the bedside for patient management! Do not just eyeball the film. It is impossible to find multiple pelvic fractures that way. Go over every arc, curve, and ring visually. If something appears possibly abnormal, compare to the other side for (a)symmetry. And if you find one break in the pelvic ring, scrutinize for more, there almost always are. Many of these are in the posterior ring, the part of the pelvis for which plain films are least sensitive. CT will help evaluate the posterior elements if feasible.
Understanding the classic LC, APC, VS mechanism classifications lend insight into when a binder will help. Realize, however, that in vehicular trauma, often the forces are multidirectional, so there will be mixed injury patterns. Ask yourself what you are trying to achieve by placing the binder. If it is closing the open book to tamponade hemorrhage, then go for it! If it is to provide some stability to a VS injury so you can move the patient without their pelvis flopping around than OK but it won't be therapeutic. If it is an LC injury where the femoral head has crushed through the acetabulum, avoid using a binder, you will only further intrude bony fragments into the pelvis!
Call IR the instant you realize there is a bleeding pelvic fracture. It takes time to prepare the suite, especially overnight!
Matt Levine, MD
Assistant Professor of Emergency Medicine
Northwestern Feinberg School of Medicine
How To Cite This Post
[Peer-Reviewed, Web Publication] Ko J, Whipple T. (2019, July 22). Pelvic Fractures. [NUEM Blog. Expert Commentary by Levine M]. Retrieved from http://www.nuemblog.com/blog/pelvic-fracture.
Other Posts You May Enjoy
References
Halawi MJ. Pelvic ring injuries: Emergency assessment and management. Journal of Clinical Orthopaedics and Trauma. 2015;6(4):252-258.
Khurana B, Sheehan SE, Sodickson AD, Weaver MJ. Pelvic ring fractures: What the orthopedic surgeon wants to know. RadioGraphics. 2014;34:1317-1333
Weatherford B. Pelvic ring fractures. Orthobullets website. https://www.orthobullets.com/trauma/1030/pelvic-ring-fractures. Accessed October 14, 2018.
Walls RM, Hockberger RS, Gauche-Hill M. (2018). Rosen's emergency medicine: Concepts and clinical practice (9th ed.). Philadelphia, PA: Elsevier/Saunders.
Murphy A, Jones J. Pelvic radiograph (an approach). Radiopaedia website. https://radiopaedia.org/articles/pelvic-radiograph-an-approach. Updated August 2018. Accessed October 14, 2018.
Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br Vol. 1988;70(1):1–12.
Singh, AP. Pelvic fractures: Presentation and treatment. https://boneandspine.com/pelvic-fractures-presentation-and-treatment/
Images:
Case courtesy of Dr Jeremy Jones, https://radiopaedia.org Radiopaedia.org. From the case https://radiopaedia.org/cases/28928" rID: 28928