Learn this helpful technique for pain control in lower extremity injuries
Resuscitative Hysterotomy
Written by: Aldo Gonzalez, MD (NUEM ‘23) Edited by: Justine Ko, MD (NUEM ‘21)
Expert Commentary by: Paul Trinquero, MD (NUEM '19) & Pietro Bortoletto, MD
Introduction
Resuscitative hysterotomy (RH) is the new term for what was previously called perimortem cesarean delivery (PMCD). The new nomenclature is being adopted to highlight the importance of the procedure to a successful resuscitation during maternal cardiopulmonary arrest (MCPA). It is defined as the procedure of delivering a fetus from a gravid mother through an incision in the abdomen during or after MCPA. The goal of the procedure is to improve the survival of the mother and the neonate.
Physiology
There are physiologic changes that occur during pregnancy which reduce the probability of return of spontaneous circulation (ROSC) during cardiac arrest. Physiologic anemia of pregnancy reduces the oxygen carrying capacity of blood and results in decreased delivery of oxygen during resuscitation. The large gravid uterus elevates the diaphragm and reduces the lung’s functional reserve capacity (FRC), which when combined with increased oxygen demand from the fetus results in decreased oxygen reserves and resultant risk for rapid oxygen desaturations. The size of a gravid uterus at 20 weeks results in aortocaval compression which reduces the amount of venous return from the inferior vena cava and reduces cardiac output during resuscitation. The theory behind resuscitative hysterotomy is to increase the probability of ROSC by reducing the impact of aortocaval compression.
Supporting Evidence
A 2012 systematic review primarily investigated the neonatal and maternal survival rates after perimortem cesarean delivery and secondarily attempted to evaluate maternal and fetal neurological outcome and the ability to perform the procedure within the recommended time frame.
Inclusion Criteria
original articles, case series, case reports and letters to the editor, and reports from databases
had minimum of least five clinical details of the case (e.g. patient age, gravidity, parity, obstetric history, medical history, presenting rhythm, or location of arrest)
AND
the care administered (chest compression, ventilation, monitoring, drug administration)
AND
maternal return of spontaneous circulation or survival to hospital discharge or fetal neonatal outcome
Exclusion Criteria
Post-delivery arrests
Studies without enough data to understand the details of the arrests
Studies with unclear maternal and fetal outcomes
Population
Pregnant woman that
(1) had a cardiac arrest or a non-perfusing rhythm
(2) received chest compression and/or advanced life support medications and/or defibrillation
Average maternal age: 30.5±6.5 years (median 32, range 17–44, IQR, 26.5–35.5, n = 80)
Gravidity: 2.5±1.5 (median 2, range 1–7, IQR 1–4, n = 59)
Parity: 1.1±1.3 (median 1, range 0–6, IQR 0–2, n = 57)
Singleton Pregnancies: 90.4% (n = 85)
Average gestational age at arrest: 33±7 weeks (median 35, range 10–42, IQR 31–39, n = 85)
Results
for cases undergoing PMCD, earlier time from arrest to delivery was associated with increased survival (p < 0.001, 95%CI 6.9–18.2)
surviving mothers: 27/57; 10.0±7.2 min (median 9, range 1–37)
non-surviving mother: 30/57; 22.6±13.3 min (median 20, range 4–60)]
for neonates delivered by PMCD/RH earlier time from arrest to delivery was associated with increased survival (p = 0.016)
surviving neonates: 14±11 min (median = 10, range = 1–47)
non-survivor neonates: 22±13 min (median = 20, range = 4–60)
Only 4 cases met the timeframe of less than minutes
Take-Aways: Performing a PMCD/RH in the 4-5 minutes time frame is difficult. However, PMCD/RH beyond the proposed time is still beneficial and earlier time to delivery from arrest is associated with better outcomes
Guideline Recommendations
Perform basic life support (BLS) in the same way as non-pregnant patients
Place patient in supine position
Left lateral decubitus (left lateral tilt) positioning is no longer recommended during compressions because of reduced efficacy of chest compressions
No modification of Chest compressions
Rate: 100-120 per minute
Depth: at least 2 inches (5 cm)
Allow for full chest recoil between compressions
Avoid interruptions as much as possible
No modification of Ventilation
Use bag-ventilation
Compression to breath ratio: 30:2 before advanced airway
Perform advanced cardiac life support (ACLS) as in non-pregnant women
No modification of Ventilation
Once breath every 6 seconds (10 BPM) with advanced airway
No modification of medications
Use 1 mg Epinephrine of epinephrine every 3-5 minutes
No modification to defibrillation
Use adhesive pads on patient
Place in anterolateral position
Lateral pad should be placed under breast tissue
Defibrillate for Ventricular fibrillation or Ventricular tachycardia
Use usual Voltages
Biphasic: 120-200 Joules
Resume compressions after shock is delivered
Special considerations during resuscitation
Obtain access above the diaphragm to minimize the effect of aortocaval compression on the administration of drugs
Perform left uterine deviation during resuscitation to reduce aortocaval compression
If a gravid patient suffers a cardiac arrest mobilize resources to prepare for the need for resuscitative hysterotomy and the resuscitation of the fetus early
Palpate the size of the gravid uterus
If above the height of the umbilicus then patient is most likely greater than 20 weeks gravid and a candidate for RH
Strongly consider performing RH (PMCD) if the patient does not achieve ROSC by the 4-minute mark and qualified staff to perform the procedure are present
Aim to have the procedure done by the 5-minute mark
Consider performing RH (PMCD) sooner if maternal prognosis is poor or prolonged period of pulselessness
RH should be performed at the site of the resuscitation
Do not delay procedure to prepare abdomen
May pour iodine solution over abdomen prior to incision
Do not delay procedure for surgical equipment if scalpel is available
Continue performing LUD while performing RH
Figure 1: One-handed left uterine deviation technique
Figure 2: Two-handed left uterine deviation technique
Steps for Resuscitative Hysterectomy
Pre-procedure
Gather supplies to perform RH
Personal Protective Equipment
Gloves
Face mask
Apron/gown
Resuscitative Hysterotomy Equipment
Scalpel(the minimum equipment to perform procedure)
Blunted Scissors
Clamps/Hemostats
Gauze
Suction
Large absorbable sutures
Needle Holder
Antiseptic Solution
Neonatal resuscitation equipment
Dry Linens
Neonatal Bag Valve Mask
Neonatal Airway supplies
Suction
Umbilical venous access equipment
Neonatal resuscitation drugs
Baby Warmer
Plastic Bag
Form teams to perform Resuscitative Hysterotomy
Resuscitative Team
Resuscitative Hysterotomy Team
Neonatal Resuscitation Team
Procedure
Maintain patient in supine position and continue compressions
Continue Left Uterine Deviation until the start of incision
Quickly prepare the skin with antiseptic solution (do not delay for skin prep)
Perform midline vertical Incision with scalpel on the abdomen from pubic symphysis to umbilicus and cut through skin and subcutaneous tissue until fascia is reached
Use fingers to bluntly dissect the rectus muscle fascia access the peritoneum (can use scalpel or blunt scissors)
Locate the uterus and differentiate it from the bladder (bladder yellow and enveloped in fatty tissue)
Make a vertical incision from the lower uterus to the fundus with scalpel (can use blunt scissors)
If the placenta is encountered while entering the uterus, cut through it
Use a cupped hand to locate the fetal part closest to pelvis
Elevate the located fetal part and pass through uterine incision while applying transabdominal pressure with other hand
Use traction and transabdominal pressure to deliver the rest of the baby
Clamp the cord at two spots and cut in between both clamps
Hand the baby to the neonatal team
Deliver placenta with gentle traction
Post-procedure
Continue performing compressions
Consider stopping if ROSC not achieved after several rounds and depending on the cause of PMCA
Give medications to promote uterine contraction
Analgesia and sedation may be required if patient achieves ROSC
Bleeding will be worse if ROSC achieved and may require pharmacologic and nonpharmacologic interventions
Closure will depend on whether the patient achieves ROSC and may necessitate careful closure to prevent further bleeding. Best performed by an obstetrician. If an obstetrician is unavailable, pack the uterus with gauze and clamps actively bleeding vessels to reduce bleeding.
Administer prophylactic antibiotics
References
Einav, S., et al. (2012). "Maternal cardiac arrest and perimortem caesarean delivery: evidence or expert-based?" Resuscitation 83(10): 1191-1200.
Jeejeebhoy, F. M., et al. (2015). "Cardiac Arrest in Pregnancy: A Scientific Statement From the American Heart Association." Circulation 132(18): 1747-1773.
Kikuchi, J. and S. Deering (2018). "Cardiac arrest in pregnancy." Semin Perinatol 42(1): 33-38.
Parry, R., et al. (2016). "Perimortem caesarean section." Emerg Med J 33(3): 224-229.
Rose, C. H., et al. (2015). "Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy." Am J Obstet Gynecol 213(5): 653-656, 653 e651.
Soskin, P. N. and J. Yu (2019). "Resuscitation of the Pregnant Patient." Emerg Med Clin North Am 37(2): 351-363.
Walls, R. M., et al. (2018). Rosen's emergency medicine: concepts and clinical practice. Philadelphia, PA, Elsevier.
Expert Commentary
This is an excellent review of an extremely rare, but potentially life-saving procedure. It may seem daunting to perform (and it should), but the evidence would say that a resuscitative hysterotomy (RH), especially if performed promptly, drastically improves survival during the catastrophic scenario of maternal cardiac arrest. This is even more important because these patients are young (and often relatively healthy) and could potentially have decades of meaningful quality of life if they can survive the arrest. That being said, this procedure is so rare that most of us not only have never performed it, but often have never even seen it. Not only that, but unlike other rare lifesaving procedures (such as cricothyroidotomy or resuscitative thoracotomy), RH is extremely difficult to practice in cadaver labs due to the unavailability of pregnant cadavers. So, we are left with the next best thing: familiarizing ourselves with the anatomy, physiology, and simplified technique of the procedure and mentally rehearsing it so that when the time comes, we can be ready.
For these rare procedures, in addition to the excellent and thorough review above, it is also helpful to simplify and rehearse the fundamental steps. I’m not an obstetrician and certainly not an expert on this procedure, but I’ve mentally prepared myself for what I would do in the event that I am faced with this grave situation and categorized it into the following simplified five step plan. Also, prior to writing this commentary I got a curbside consult from a friend from med school and actual obstetrician and gynecologic surgeon, Dr. Pietro Bortoletto.
First off, the indications-- basically, a pregnant woman estimated to be >20 weeks EGA who has suffered a cardiac arrest. Don’t worry about the 4 minutes, make the decision to perform a RH right away and start prepping. Delegate someone to call the appropriate resuscitation teams if available. Then start the procedure.
Step 1: Setup. You probably don’t have a c section kit in your trauma bay, so instead open the thoracotomy tray and you’ll have most of what you need. Go ahead and set aside the finochietto rib spreaders so that you don’t have a panic attack trying to remember how to put those together with other people watching. But everything else you’ll need will be in that tray (basically a scalpel, blunt scissors, and hemostats).
Step 2: Cut into the Abdomen. Splash prep the abdomen with betadine. Then make your long vertical incision from the uterine fundus to the pubic symphysis. Cut through the skin and subcutaneous tissue then bluntly separate the rectus and enter the peritoneum with scalpel or blunt scissors. Extend the peritoneal incision with blunt scissors.
Step 3: (carefully) Cut into the Uterus. First, locate the uterus. Then, take a deep breath and remember that there is a fetus inside the uterus. With that terrifying thought in mind, cut vertically into the uterus, insert your fingers, and extend the incision upwards with blunt scissors and a steady hand. If you encounter an anterior placenta, cut right through it.
Step 4: Delivery. Deliver the fetus either by cupping the head and elevating it through the incision or by grabbing a leg, wiggling out the shoulders, and then flexing the head. Hand over the neonate to whoever is taking the lead on the neonatal resuscitation (will need to be warmed, stimulated, and potentially aggressively resuscitated). Clamp and cut the cord, leaving a long enough umbilical stump for an easy umbilical line if needed. Then using gentle traction, attempt delivery of the placenta. If it isn’t coming easily, leave it alone so as not to stir up more bleeding.
Step 5: Extra credit. If you’ve made it this far as an emergency physician and there is still no obstetrician in sight, you can continue resuscitation, focusing on stopping the uterine bleeding. While you don’t need to close the fascia or skin, it can be helpful to close the uterine incision to prevent additional blood loss. You can do this with a whip stitch using 0-0 vicryl (or if that seems like showing off, you can just pack it with sterile gauze. If you’ve got it handy, give 10 IU oxytocin to stimulate uterine contraction and further slow bleeding. Feel free to order some antibiotics as well. Otherwise, continue maternal resuscitation following typical ACLS.
The big picture here is that this is a heroic, potentially life-saving procedure that most of us will never do. But we can all take a few minutes to read an excellent review like the blog post above, watch a video, and mentally walk ourselves through the simplified steps. That preparation will afford us some much-needed confidence if we are ever faced with this terrifying scenario.
Paul Trinquero, MD
Medical Director
Department of Emergency Medicine
US Air Force Hospital - Langley
Pietro Bortoletto, MD
Clinical Fellow
Reproductive Endocrinology & Infertility
Weill Cornell Medical College
How To Cite This Post:
[Peer-Reviewed, Web Publication] Gonzalez, A. Ko, J. (2021, Dec 13). Resuscitative Hysterotomy. [NUEM Blog. Expert Commentary by Trinquero, P and Bortoletto, P]. Retrieved from http://www.nuemblog.com/blog/resuscitative-hysterotomy.
Other Posts You May Enjoy
Scalpel Finger Bougie
Written by: Em Wessling, MD (NUEM ‘22) Edited by: Therese Whipple (NUEM ‘20) Expert Commentary by: Joseph Posluszny, MD
Expert Commentary
Establishing an airway via a cricothyroidotomy is a stressful and tense experience. In almost all of these cases, experienced airway staff have already attempted advanced airway maneuvers in patients typically at high risk for inability to intubate. As the oxygen saturation drops and the patient becomes unstable, the most adept proceduralist present (whether emergency department physicians or surgeons) are asked to step in to secure a surgical airway.
The scalpel-finger-bougie technique is one proven and reliable method to secure a surgical airway via a cricothyroidotomy. Some additions to the technique described above are:
Use a vertical incision through the skin and soft tissues. If you are too superior or inferior with your initial incision, then this incision can be easily extended as needed. A horizontal incision commits you to that cranial-caudal level. It is often more of a struggle to identify the cranial-caudal orientation of the cricothyroid membrane rather than the medial-lateral orientation.
In a patient with a stable and flexible neck, retract the neck via cranial pressure on the chin to bring the neck structures better into your working field. Insert a shoulder roll if available (unlikely) to augment this positioning.
After the tube is advanced, listen for bilateral breath sounds. It is common, in this adrenaline fueled procedure, to advance the endotracheal tube too far, leading to a right main stem intubation. This can limit your ventilation and oxygenation and can lead to confusion about the airway placement in the neck. If there are no left lung field breath sounds, then pull the tube back until bilateral breath sounds are confirmed with auscultation.
Always verify tube placement with capnography.
Persistent, moderate volume bleeding is often from injury to the anterior jugular vein. Gentle, directed pressure on the area can control this bleeding while the patient is being transported to the operating room for a more definitive airway.
Joseph Posluszny, MD
Assistant Professor of Surgery (Trauma and Critical Care)
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Wessling, E. Whipple, T. (2021, Aug 2). Scalpel Finger Bougie. [NUEM Blog. Expert Commentary by Posluszny, J]. Retrieved from http://www.nuemblog.com/blog/scalpel-finger-bougie
Other Posts You May Enjoy
Felon
Written by: Daniel Levine, MD (NUEM ‘23) Edited by: Will LaPlant, MD, MPH (NUEM '20) Expert Commentary by: Matt Levine, MD
Expert Commentary
Thank you for the handy concise reference for felon management. Some key points of emphasis and elaboration:
A TENSE distal finger pad is what distinguishes a felon from other finger infections. A paronychia can be the portal of entry (as in this case https://www.ortho-teaching.feinberg.northwestern.edu/cases/hand/case14/index.html) . However, a paronychia alone should not cause a TENSE finger pad so check the finger pad before diagnosing a finger infection as a simply a paronychia. Flexor tenosynovitis is not localized to the distal pad and should be readily distinguishable from a felon, which is localized. Whitlow may be confused for a purulent infection but is cutaneous and again, will not have a TENSE pad.
The felon itself is an intense throbbing pain and the procedure is extensive so analgesia is a major point of emphasis for successful management.
The key to understanding the nature and treatment of a felon is knowledge of the anatomy of the distal finger. There are 15-20 discrete, noncompliant, tough fibrous septae of the finger pad which run from the periosteum to the skin. The abscess of a felon affects these unforgiving septae, which is why is it so painful. The incision must enter the septae and the dissection must break up the remaining septae to completely drain the infection. Other abscesses we drain may have loculations but not the tough septations of a felon. So the dissection must be firm enough to break these septations.
There are many different (and interestingly named) incisions that have been described to decompress a felon, like the “hockey stick” (https://lacerationrepair.com/felon-hockey-stick/) or the “fish mouth” (https://lacerationrepair.com/felon-fish-mouth/). Many sources prefer lateral approaches over volar approaches. The volar approaches incise directly through the highly innervated pad and residual paresthesia affecting finger function is a concern.
Be aware that you are dissecting just volar to the phalanx to get into these septae, so this is deep. If the etiology of the felon is direct extension from a paronychia, drain the paronychia first and see if you can access the felon by dissecting through the paronychia tract. Afterwards, insert packing or a drain. I have even seen consultants make bilateral incisions and feed a drain all the way through to facilitate drainage.
Refer all of these patients to hand clinic. One patient I had who was lost to follow up returned to the ED weeks later with osteomyelitis of the distal phalanx (https://www.ortho-teaching.feinberg.northwestern.edu/cases/bone-lesions/case4/index.html).
Matthew R Levine, MD
Associate Professor of Emergency Medicine
Northwestern Memorial Hospital
How To Cite This Post:
[Peer-Reviewed, Web Publication] Levine, D. LaPlant, W. (2021, March 8). Felon. [NUEM Blog. Expert Commentary by Levine, M]. Retrieved from http://www.nuemblog.com/blog/felon.
Other Posts You May Enjoy
Pericardiocentesis
Written by: David Feiger, MD (NUEM ‘22) Edited by: Abiye Ibiebele, MD (NUEM ‘21) Expert Commentary by: Daniel Schimmel, MD, MS
Introduction
An emergent pericardiocentesis may be a life-saving procedure and is indicated in patients with pericardial effusion and associated hemodynamic instability. The degree of pericardial effusion severity lies on a continuum and when associated with hemodynamic instability, is known as cardiac tamponade. The volume and rate at which the effusion develops most affects a patient’s hemodynamics. The clinical exam findings – hypotension, distant heart sounds, and jugular venous distention (known as Beck’s Triad) – often do not occur simultaneously if cardiac tamponade is suspected and confirmed early.
Given the urgency of the situation and severity of the patient’s clinical status, blind insertion of a needle into the pericardial space using anatomic landmarks has historically been the method of choice to restore hemodynamic stability. The availability of bedside ultrasound in many emergency departments more recently has led many physicians to pursue an image-guided pericardiocentesis. Various studies have demonstrated decreased mortality and morbidity with an ultrasound-guided approach when compared to a blind approach. However, depending on the clinical context and tools available, a blind approach may be the optimal choice.
Indications and Contraindications
Hemodynamic instability secondary to pericardial effusion, is the number one reason to perform an emergent pericardiocentesis in the emergency room. Pericardiocentesis for patients with symptomatic pericardial effusion but without hemodynamic instability may be deferred to inpatient management.
An emergent pericardiocentesis has few contraindications. Aortic dissection or cardiac free wall rupture is sometimes considered an absolute contraindication to pericardiocentesis, but in the absence of immediately available life-saving procedures, pericardiocentesis should be strongly considered. Relative contraindications include use of anticoagulation, platelets < 50K, and uncorrected coagulopathy. Furthermore, trauma patients with hemopericardium should preferentially undergo surgical pericardial drainage or emergency thoracotomy.
Blind Emergent Pericardiocentesis
Relevant Anatomy to Keep in Mind
Internal thoracic artery (internal mammary artery) – artery running cephalad to caudal on the anterior chest wall parallel to the sternum bilaterally
Neurovascular bundle – a collection of an intercostal vein, artery, and nerve running caudal to each rib
Materials
Sterile gloves, gown
Chlorhexidine swab
At least a 7 cm 18-gauge spinal needle or introducer needle if planning for continuous access to pericardial space
Syringes (10mL and 60-80mL)
Three-way stopcock
Plastic drainage tubing
Surgical clamp (optional)
1) Position the patient appropriately.
Provide respiratory support with nasal cannula or mechanical ventilation as indicated. Placing patients upright at 30 degrees to enhances comfort and allows gravity-dependent pooling of pericardial fluid.
2) Select an entry site.
Left parasternal and apical approaches are the most commonly pursued and have been shown to be superior to the classic subxiphoid approach in observational studies. When selecting an entry point, recall the location of the internal thoracic artery and subcostal neurovascular bundle. Cleanse a large area of the chest and upper abdomen with the chlorhexidine swab.
3) Insert and advance the spinal needle.
Insert the spinal needle into skin. Once the bevel is in the skin, remove the stylet, attach a three-way stopcock with a large volume syringe attached and maintain negative pressure as you advance the needle. Avoid sliding the needle laterally to prevent lacerating tissues. If a different trajectory is required, retract the needle, keeping the bevel in the skin and drive the needle at the desired angle maintaining negative pressure on the syringe. Momentary resistance may be met as the needle approaches the pericardium, but with continued advancement, a “pop” may be felt followed by aspirate in the syringe and improving patient hemodynamics. See below for more detailed instructions for each approach.
Subxiphoid
Insertion: 1 cm inferior to the left xiphocostal angle, 30 degrees with the patient’s chest
Direction: Towards left mid-clavicle. If unsuccessful, retract the spinal needle and redirect 10 degrees towards the patient’s right
Parasternal
Insertion: Fifth intercostal space at the left parasternal border no more than 1 cm lateral, cephalad to the inferior rib and perpendicular to the patient’s chest
Direction: Posterior
Apical
Insertion: Fifth, sixth, or seventh left intercostal space approximately 6 cm from the parasternal border, cephalad to the inferior rib
Direction: Patient’s right shoulder
4) Draining the pericardial effusion.
Steady the needle with a surgical clamp at the needle shaft closest to the surface of the skin effectively preventing further needle advancement. Attach the plastic tubing to the stopcock allowing emptying of the syringe contents into a collecting vestibule without exchanging syringes. If planning to place a more permanent line (see “Establishing Continuous Access to the Pericardial Space”), consider aspirating just enough fluid to stabilize the patient’s hemodynamics and leave the remaining pericardial fluid to provide space for placing a line.
Tips for Pericardiocentesis with Ultrasound Guidance
Additional materials:
Bedside ultrasound
Sterile ultrasound probe cover
Skin marker
The safety and success of the steps above can be enhanced with bedside ultrasound. Bedside ultrasound can help prior to the procedure by finding the largest effusion nearest the skin and during the procedure by visualizing the needle trajectory in order to avoid important organs and other structures. There are several methods of ultrasound use in pericardiocentesis.
In static guidance, ultrasound is only used for procedure planning. The subxiphoid, parasternal, and apical views can be explored to find the largest effusion and determine the optimal entry. Often, the needle entry point is marked with a skin marker and another mark is made for the planned trajectory. Distance and angle from the skin to the effusion is also noted.
In dynamic guidance, the needle is passed through the skin parallel to the 2D plane created by the ultrasound probe after finding an effusion pocket. The needle can be visualized as it is advanced towards the pericardial effusion and enters the pericardial space.
No ultrasound? Hook up an EKG!
Additional materials:
Continuous EKG monitor
Wire with alligator clips
A continuous EKG can be used to prevent inadvertent traversing of the myocardium with the needle without an ultrasound. Attach one alligator clip to the needle and the other to an anterior lead on a continuous EKG. ST-elevations will be apparent on the EKG if the myocardium is touched. If ST-elevations are noted, simply retract the needle.
Confirmation of Pericardial Access with Ultrasound Guidance
Additional materials:
Bedside ultrasound
Two 10 mL syringes (one with 4 mL of saline, one with 0.5 mL of air)
Confirming success in accessing the pericardial space can also be made injecting agitated saline and visualizing bubble artifact on ultrasound. To do so, attach the two saline syringes to the three-way stopcock. Turn off access towards the patient and rapidly push the contents from one syringe to the other until the fluid appears opacified. When all the saline is in one syringe, close off the access to the empty syringe and push the fluid towards the patient, visualizing it on the ultrasound. Confirmation is especially important when blood is aspirated and helps distinguish between pericardial versus ventricular placement.
Establishing Continuous Access to the Pericardial Space
Additional materials:
Flexible or curved-tip (J) guidewire
6-8 Fr drainage catheter (pigtail, sheath, or central venous catheter)
7 cm or longer 18-gauge introducer needle (as opposed to spinal needle)
Dilator
11 blade scalpel
Suture
Needle driver
Many of the materials above may be found in a central venous kit. Using the Seldinger technique, a line can be placed for continuous access to the pericardial space. Ensure that an introducer needle is used when initially accessing the pericardial space. Keeping the surgical clamp and needle in place, remove the stopcock and syringe, and gently advance the guidewire just beyond the bevel of the needle. Remove the introducer needle, ensuring the guidewire does not move, and use the scalpel to make a short incision at the guidewire’s entry into the skin. Advance the dilator over the guidewire to loosen the tissue. Remove the dilator leaving the guidewire in place and advance the drainage catheter just 1 cm beyond the guidewire into the pericardial space. Retract the guidewire while maintaining the position of the catheter, aspirate fluid to confirm placement, and secure the drain’s position with sutures and placement of a sterile dressing. Further confirmation of proper placement can be made using the agitated bubble study as described in “Confirmation of Pericardial Access with Ultrasound” above.
Conclusion
There are very few contraindications for an emergent pericardiocentesis in a patient with pericardial effusion and hemodynamic instability. While ultrasound-guided pericardiocentesis have lower morbidity and mortality rates, clinical context and emergent patient decompensation may make an image-guided procedure infeasible. Apical and parasternal access with a blind procedure have fewer complications than a subxiphoid approach. A pericardiocentesis may be a life-saving intervention as even a small amount of fluid aspirated may dramatically improve a patient’s hemodynamics.
Expert Commentary
Thank you Dr. Feiger for this excellent summary of pericardiocentesis. From center to center there can be variability in the expertise and mechanism through which pericardiocentesis is performed. Some institutions may have an echo focused pericardiocentesis service, while some institutions may perform the bulk of their pericardiocentesis in an interventional suite with the assistance of fluoroscopic imaging. However, there are times when pericardiocentesis must be performed as an emergency procedure with landmark guidance. Luckily, point of care ultrasound has been very commonplace in the emergency department and intensive care units facilitating visualization of fluid pockets that can be identified for safer access and to demonstrate successful drainage at the end of the procedure.
The relevant anatomy and associated complications from tissue injury during needle advancement for pericardiocentesis changes depending on the planned access route.
Subcostal
Liver laceration or puncture
Pneumothorax
Right atrial or ventricular laceration
Apical
Pneumothorax
Left or right ventricular laceration
Parasternal
Pneumothorax
Right ventricular laceration
In each location, careful use of ultrasound can avoid potential life-threatening complications. How the ultrasound is used also varies depending on location. Generally the ultrasound can be used to identify a path and I will have trainees hold the ultrasound the exact same way as they would hold their needle to mimic the path they will use when advancing into the pericardial space.
Common errors that I have seen are listed below.
Moving the needle side to side while it is in the body to try and find the appropriate space. I am impressed at the body’s ability to tolerate a straight in and out movement of a needle. But moving a needle tip back and forth creates lacerations that are difficult to heal and may result in tissue damage and uncontrollable bleeding requiring surgical intervention.
Moving the needle to find it under ultrasound, rather than moving the probe to find the needle can be dangerous. If the needle is in the wrong location, it should be moved. Otherwise, do not bounce the needle within the body to try and identify it on ultrasound.
A common subcostal error is needle path facing towards the spine through the torso. The subcostal position can be more successful with the patient upright at 30 degrees so that the fluid layers to the bottom portion of the heart, increasing the pocket size for needle entry. However, this position then requires the physician to aim slightly up, almost moving parallel to the ribs, to avoid needle entry being too low and passing underneath the effusion.
Also from the subcostal position, the initial position angle for subcostal pericardiocentesis should be to the left middle cervical bone as Dr. Feiger mentioned. However, many performing subcostal pericardiocentesis overcompensate initially and head too laterally to capture fluid.
From the apical position, the fluid is likely best obtained with the patient in the left lateral decubitus position. A drop door that is often present on an sonographer’s bed for performing echocardiograms is nice but not necessary.
As mentioned, the cardiac probe is not generally used to watch needle entry but to identify the most optimal path. However, if also equipped with a vascular probe, in the parasternal location, the vascular probe can easily watch the needle enter into the pericardial space while avoiding delicate structures like the internal thoracic artery.
Using fluoroscopic guidance, needle location can be identified in relation to the movement of the cardiac border and wire advancement can be used to identify a course consistent with the pericardial space and not limited by other cardiac structures. A small amount of contrast can be injected into the space and seen to highlight the cardiac borders allowing confirmation of the pericardial space.
But in the absence of fluoroscopy, and a more specific confirmation, an echo with agitated bubbles injected can verify presence of the needle, or a microcatheter, in the pericardial space. If after injection, bubbles are seen within the cardiac chambers, the needle should be withdrawn. If possible to obtain a pressure measurement during the procedure, this is one other guide to inform the operator of the needles location. If a right ventricular waveform Is present, the needle has entered the ventricular space. It may be possible to withdraw the needle until the high pressures of the ventricle reduce and if the needle aspirates, another agitated bubble injection can be performed.
An urgent pericardiocentesis with a large effusion can be easily performed at the bedside, particularly with the aid of an ultrasound and knowing the anatomy with immediate improvement in hemodynamics. Send the fluid for analysis and exchange the needle for a drain to ensure patient stability until the evaluation is complete.
Daniel Schimmel, MD, MS
Interventional Cardiologist
Northwestern Memorial Hospital
Associate Professor
Feinberg School of Medicine
How To Cite This Post:
[Peer-Reviewed, Web Publication] Feiger, D. Ibiebele, A. (2021, Feb 8). Pericardiocentesis. [NUEM Blog. Expert Commentary by Schimmel, D]. Retrieved from http://www.nuemblog.com/blog/pericardiocentesis.
Other Posts You May Enjoy
References
Gueria, Rajesh. “Ultrasound Guided Procedures in Emergency Medicine Practice - Pericardiocentesis.” Sonoguide, 2008, www.acep.org/sonoguide/pericardiocentesis.html.
Heffner, Alan C. “Emergency Pericardiocentesis.” Edited by Allan B Wolfson et al., UpToDate, 29 May 2019, www.uptodate.com/contents/emergency-pericardiocentesis?search=pericardiocentesis&source=search_result&selectedTitle=1~65&usage_type=default&display_rank=1.
Konnoff-Phillips, Kelly and Janis Provinse, directors. Agitated Saline Bubble Study. Highland Hospital Emergency Department, 2015.
Maisch, Bernhard, and Sabine Pankuweit. Interventional Pericardiology: Pericardiocentesis, Pericardioscopy, Pericardial Biopsy, Balloon Pericardiotomy, and Intrapericardial Therapy. Springer, 2011.
Nicks, Bret A, et al. Emergency Pericardiocentesis. New England Journal of Medicine, 22 Mar. 2012, www.nejm.org/doi/full/10.1056/NEJMvcm0907841.
Ultrasound Guidance for Lumbar Puncture
Written by: Maurey Hajjar, MD, MPH (NUEM ‘22) Edited by: Justin Seltzer, MD (NUEM ‘21) Expert Commentary by: Alex Ireland, MD (NUEM '20)
Expert Commentary
Thank you to Dr. Hajjar and Dr. Seltzer for their excellent review of an underutilized ultrasound procedure.
After several challenging lumbar punctures during my residency training, I began to adopt this technique as a supplemental tool to improve first-pass success. When beginning, the patient can be placed in either the lateral decubitus or the upright position. However, I have found that in the patients for whom you are looking for ultrasound guidance, the anatomy due to body habitus is already challenging, and upright positioning offers the best advantage of maintaining midline.
There are several approaches to identifying your target with ultrasound, and my preferred strategy is different than the one mentioned in this post. After palpating the bilateral anterior superior iliac spines and drawing lines inward towards the midline, I start with my probe in the transverse view to identify the spinous processes at L3, L4, and L5. I mark above and below my probe at each process to identify the midline.
I then rotate the probe 90 degrees into a longitudinal view, but I keep my probe in the midline to identify contiguous vertebral spinous processes and the intervertebral or interspinous spaces between them. I place a mark on both sides of my probe with it aligned in the middle of this intervertebral space, which will be the exact insertion point of my needle.
Another key advantage of ultrasound is the ability to measure the anticipated depth of needle insertion. After identifying the spinous processes and intervertebral space in longitudinal view, I increase the depth and the gain to view the mixed echogenicity soft tissue and ligaments, and then see the hypoechoic subarachnoid space underneath the dura mater. I measure the depth of this space and then have an estimate of how far to insert the needle before obtaining cerebrospinal fluid.
Lastly, I would highly recommend attempting this technique on several “easy” patients where you can also readily palpate the anatomy. Similar to using a bougie during difficult intubations, we need to be skilled with our rescue techniques through diligent preparation and repeated practice.
References
Ultrasound Guided Lumbar Puncture. MGH Ultrasound.
Alex Ireland, MD
Emergency Medicine Physician
Vituity Group
Chicago, IL
How To Cite This Post:
[Peer-Reviewed, Web Publication] Hajjar, M. Seltzer, J. (2020, Dec 7). Ultrasound Guidance for Lumbar Puncture. [NUEM Blog. Expert Commentary by Ireland, A]. Retrieved from http://www.nuemblog.com/blog/ultrasound-imaging-for-lumbar-puncture
Other Posts You May Enjoy
Temporomandibular Joint Reductions
Written by: Trish O’Connell, MD (PGY-2) Edited by: Jacob Stelter, MD (PGY-3) Expert commentary by: Matt Levine, MD
Expert Commentary
That was a high yield visual guide to TMJ reductions. Earlier in my career I was often frustrated by these cases. I was taught the traditional reduction method. I found myself having to sedate the patient and stand on the bed to generate enough downward force. This was awkward and I was still usually unsuccessful. The wrist pivot method really changed my practice. I found it required less sedation, easier to generate force without awkward positioning, required less physical strength, and led to higher success rates for me. My current practice is to have a patient roll a 10mL syringe in their mouth while I am setting up, which usually doesn’t work, and to proceed with the wrist pivot technique if still dislocated.
While procedural sedation has evolved away from versed and more towards agents such as ketamine, etomidate, and propofol, versed remains an ideal agent for TMJ reduction. It provides good anxiolysis and is a better muscle relaxant than etomidate and ketamine. The deep sedation of propofol is unnecessary.
When the sedated patient awakens, beware of “the yawn”! I’ve had patients dislocate again that way, to the chagrin of the patient (and the benefit of the procedure-seeking resident). Wrapping Kerlex gauze under the chin and around the top of the head until the patient is alert enough to avoid full yawning will prevent “the yawn.”
The main role of imaging is to rule out associated fracture. Plain films are generally inadequate to confirm or rule out TMJ dislocation. If you really need imaging, CT is the best test. If the patient had no trauma but their mouth is stuck open, you usually won’t need imaging.
Matthew R. Levine, MD
Assistant Professor
Department of Emergency Medicine
Northwestern University
How to Cite this Post
[Peer-Reviewed, Web Publication] O’Connell, T, Stelter, J. (2020, Mar 2). Temporomandibular Joint Reductions. [NUEM Blog. Expert Commentary by Levine M]. Retrieved from https://www.nuemblog.com/blog/tmj-reduction
Other posts you may enjoy
Bougie Journal Club
Written by: Amanda Randolph, MD (NUEM PGY-3) Edited by: Katie Colton, MD (NUEM ‘19) Expert commentary by: Howard Kim, MD
Introduction:
Endotracheal intubation is one of the most common and life-saving procedures performed in the Emergency Department (ED), though it is not without risk – approximately 12% of ED intubations result in an adverse event. First-pass success has been linked to improved outcomes, but in the case of a difficult airway, this goal can be challenging. The bougie is typically reserved as a rescue device in these situations. However, a study recently published in JAMA questions this approach, and instead asks whether the routine use of a bougie during all difficult airway attempts would improve first-pass success.
The Study:
Driver BE, Prekker ME, Klein LR, et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA. 2018;319(21):2179–2189. doi:10.1001/jama.2018.6496
Study Design:
This study was a randomized clinical trial performed at Hennepin County Medical Center, an urban academic Emergency Department.
Population:
Investigators enrolled consecutive patients 18 years and older whom the attending emergency physician planned to intubate using a Macintosh laryngoscope blade (direct or video).
Exclusion criteria included known anatomic distortion of the upper airway (ie angioedema, epiglottitis, laryngeal mass, or malignancy), as the bougie has already been proven more effective in these patients in previous studies. Prisoners and pregnant patients were also excluded.
After intubation, the physician recorded whether any difficult airway features were present: body fluids obscuring the laryngeal view, airway obstruction or edema, obesity, short neck, small mandible, large tongue, facial trauma, or cervical spine immobilization. Patients were then subcategorized based on the presence of 1 or more difficult airway characteristics.
Intervention Protocol:
To optimize a balanced study population, eligible patients were first sorted into 2 strata – those with obesity or cervical immobilization, and those without these features. From that point, patients from each stratum was randomized 1:1 to either bougie or endotracheal tube (ET tube) + stylet for the first attempt.
The intubating physician was free to direct the procedure as they saw fit, including patient positioning, pre-oxygenation, the use of RSI, and cricoid pressure. The physician could choose between direct laryngoscopy using a Macintosh blade, or video laryngoscopy using a C-MAC or GlideScope. If video laryngoscopy was chosen, the physician could elect whether to view the video screen.
In the bougie group, the physician inserted the bougie into the trachea, an assistant loaded the ET tube, and the operator guided the tube through the vocal cords. If resistance was met, the physician retracted the tube 2cm, rotated 90 degrees and re-advanced.
In the ET tube + stylet group, a straight to cuff shape was used. If resistance was encountered, the physician could reshape the tube/stylet as needed.
If intubation was unsuccessful on the first attempt, the physician was free to change any equipment or devices. Correct tube placement was determined by waveform capnography.
Outcome Measures:
Primary outcome: first-pass intubation success
Successful intubation on the first laryngoscopy attempt with device as previously randomized (bougie or ET tube)
Secondary outcomes:
Hypoxemia (sat < 90%, or > 10% desat during intubation if already hypoxemic)
First attempt time elapsed (laryngoscope insertion to removal)
Esophageal intubation
Results:
In patients randomized to the bougie arm, there was a 14% absolute increase in the rate of first-pass success in patients with at least one difficult airway feature (96% vs 82% bougie vs ET tube +stylet).
The bougie approach was superior in subsets of patients with predictors of airway difficulty including C-spine immobilization, obesity, and Cormak-Lehane grades 2-4.
Even in patients not predicted to have a difficult airway, there was a 7% absolute increase in first-pass success with the bougie approach (99% vs 92% with ET tube + stylet).
There was a small but significant increase in the time elapsed on first-pass success with the bougie (38 seconds) vs ET tube + stylet (34 seconds).
A more extensive summary of the results is depicted in Table 3:
Interpretation:
This study concludes that the bougie improves first-pass success rate both in difficult airways and standard airways. The small increase in time to first-pass success when using a bougie is outweighed by the need to fall back on rescue techniques more frequently when starting with an ET tube and stylet. Therefore, authors propose the use of a bougie as a routine primary intubation device for all patients. This argument is compelling and potentially practice-changing. Most EDs including NMH have adopted the practice of using a bougie right away when there is an obviously difficult airway (laryngeal mass, neck hematoma etc), but otherwise the bougie is often reserved for backup after one or more failed attempts. This relies on a perhaps now invalid model of an algorithmic approach to the difficult airway in which operators progress through a series of rescue devices and maneuvers. In light of this study, it may be time for a culture shift in EM toward routine bougie use.
Strengths:
This is a well-designed randomized controlled trial, with a total of 752 patients studied, generating enough power to provide meaningful results. The methodology of using the bougie and the ET tube + stylet was highly standardized. At the same time, the physicians were free to direct the remainder of the intubation strategy, including preoxygenation, medications, patient positioning, operator training, laryngoscope type, and video assistance. This is a realistic approach that would be generalizable to the typical ED experience. The power of this study was sufficient to then create subgroup analyses for each of these factors, and prove they were not confounders.
Weaknesses:
This study is primarily limited by its single center design and thus may not be generalizable to all Emergency Departments. This particular hospital had been using the bougie routinely prior to this study, which is uncommon. This may have led to overestimation of the bougie’s benefit. Further studies involving multi-centered trials are needed to affirm generalizability. Finally, this study by design could not be blinded, which could have led to biased results.
Take Home Points:
This was a single center randomized controlled trial of bougie vs ET tube + stylet for first-pass intubation
The bougie was significantly more effective in all patients, with or without difficult airway features
This study is potentially practice-changing and suggests the bougie should be used as a routine primary intubation device for all patients in the ED
Further studies including a multi-centered trial would be helpful to affirm generalizability
Expert Commentary
Thank you for the excellent review of this randomized trial of a bougie-first intubation strategy. I agree that this study is potentially practice-changing, with the important caveat that your initial mileage may vary due to the study setting of a single ED with an existing culture of utilizing the bougie. Still, the demonstrated 11% absolute difference in first-pass success among all-comers (including patients with and without difficult airway characteristics) is compelling.
Intuitively, routine use of the bougie should be a familiar concept to ED physicians. We regularly utilize Seldinger technique in the placement of various vascular access devices, and the bougie can be thought of as the Seldinger technique of the airway. Anecdotally, I feel that the primary benefits of the bougie are improved visualization of the glottic inlet and tactile feedback from tracheal clicks and holdup. Many of us will encounter airways that we do not initially perceive to be difficult based on anatomic features (e.g., non-obese, reassuring Mallampati) only to be perplexed by the visual appearance of the glottic inlet after blade placement (see Kovacs et al., 2017) or complete obscuring of the glottic inlet by rapidly re-accumulating blood or vomitus. In these scenarios, tactile feedback can be reassuring of proper tube placement.
Importantly, use of the bougie requires the operator to understand three key points: first, many novice users instinctively remove the intubating blade after the bougie is placed but prior to railroading the endotracheal (ET) tube over the bougie; this makes ET tube placement difficult but can be addressed by re-inserting the intubating blade (and confirming that the bougie remains in the correct position). Second, as the study authors point out, the bevel tip of the endotracheal tube can get caught on the arytenoids. This can be addressed by rotating the ET tube and re-attempting insertion. Finally, bougie placement can be difficult with hyper-angulated devices, such as the traditional GlideScope blade or the “D-Blade” for the C-MAC – hence the reason for excluding these devices in the trial. These hyper-angulated devices require the ET tube (and bougie) to navigate a hyper-acute angle for delivery, which is why they come with a special hyper-angulated metal stylet.
Finally, while I am an advocate of a bougie-first intubation strategy, I would emphasize that it is important not to become too infatuated with or dependent on a single airway technique. For example, a bougie cannot solve the dilemma of a small, restricted mouth that will not accommodate blade placement (e.g., advanced scleroderma), nor will it allow you to navigate an edematous tongue that occludes the entire oropharynx (e.g., severe angioedema). The best airway technicians are facile in a number of airway techniques, are always cognizant of the potential for their primary approach to be unsuccessful, and have a clear algorithm for how to respond to potential obstacles. This requires learning as many airway techniques as possible during your training (e.g. video, direct, LMA, bougie, fiber-optic).
References:
Kovacs G, Duggan LV, Brindley PG. Glottic Impersonation. Can J Anaesth. 2017 Mar;64(3):320. PMID 28028675.
Howard S. Kim, MD MS
Assistant Professor
Department of Emergency Medicine
Northwestern University Feinberg School of Medicine
How To Cite This Post
[Peer-Reviewed, Web Publication] Randolph A, Colton K. (2019, Nov 25). Bougie Journal Club. [NUEM Blog. Expert Commentary by Kim H]. Retrieved from http://www.nuemblog.com/blog/bougie.
Other Posts You May Enjoy
Procedural Sedation
Written by: Mike Conrardy, MD (NUEM PGY-3) Edited by: Will LaPlant, MD (NUEM PGY-4) Expert commentary by: Seth Trueger, MD, MPH
I Want to be Sedated…
Mastering Procedural Sedation in the Emergency Department
Procedural sedation, which is not called conscious sedation given the goal is to ensure the patient is not fully conscious, comes in a variety of flavors. Propofol, ketamine, or “ketofol” (the two used together) are typically preferred by emergency physicians, yet there are other options that may be more appropriate depending on the circumstances. In this article, we will provide a brief overview of the basics of procedural sedation, then dive deeper to provide more information about the specific agents that can be used for procedural sedation, including the pros and cons of each.
How many people are necessary to perform procedural sedation?
Generally it is recommended to have three personnel for procedural sedation (typically at least one doctor to perform the procedure and two other providers to provide sedation and monitor the patient), although using two providers (one doctor and one nurse) has been shown to have a similar complication rate.
What type of monitoring is necessary during the procedure?
Monitor vitals, telemetry, SpO2, EtCO2, and the patient’s level of sedation by physical exam. I prefer having EtCO2 if it is available, although remember EtCO2 can lead to false positives (e.g. suspected apnea when apnea is not present), but also provides earlier recognition of hypoventilation.
What other supplies should I have ready?
Oxygen by face mask has been shown to reduce likelihood of hypoxemic episodes. In addition to the above monitoring equipment, at the bedside you should have a bag-valve-mask, oral airway, nasal airway, suction, and intubation supplies ready in case they are needed. A good acronym for remembering all the supplies is SOAP ME: Suction, Oxygen, Airway equipment, Preoxygenation, Monitoring, Medications, ETCO2. As with most procedures, preparation is the most important step.
What are the most common complications of procedural sedation?
Aspiration (<2%), intubation (<2%), laryngospasm (<5%), nausea/vomiting (<5%), respiratory depression (10-20%), hypotension (10-20%), and emergence reactions if using ketamine (up to 20%).
What if my patient is pregnant?
Unfortunately, we have limited data on the safety of procedural sedation in pregnant patients. We do know that pregnant patients are more prone to hypoxemia, can be more difficult to intubate due to physiologic changes to the airway, and have a higher risk of aspiration when sedated after 16 weeks of pregnancy. Clinicians must weigh the risks and benefits of performing sedation in a pregnant patient, but if a procedure is emergent, delay is not a reasonable option. To reduce the risk of aspiration, utilize left lateral decubitus positioning and consider using pre-procedural metoclopramide and antacids.
Etomidate, propofol, and ketamine may all have an impact on brain development in pregnancy, but evidence in pregnancy is limited for all these medications and they have not been shown to be teratogenic. Propofol may be preferred given it is short acting and is used commonly for general anesthesia in pregnancy. Given that some benzodiazepines have been shown to be teratogenic, midazolam should not be used.
Prior to giving a sedating agent, is pretreatment necessary?
It is not necessary, but using ondansetron or another antiemetic prior to sedation may reduce vomiting and aspiration (and is at least generally safe and uncomplicated). Midazolam may also useful in conjunction with ketamine to reduce some of the post-sedation side effects, i.e. agitation and emergence reactions, although increases the risk of respiratory depression. More specifics are described below.
After sedation, when can a patient be discharged?
Once a patient is back to their neuromuscular and cognitive baseline, typically 30 minutes after the procedure, they can go home. Our practice is to PO trial a patient prior to discharge and ideally have them go home with a friend or family member who can monitor them at home for a few hours.
Agents:
Propofol:
Onset/Duration: Onset of ~40 seconds, duration of ~5 min.
Dose: 0.5 – 1 mg/kg loading dose followed by 0.5 mg/kg doses every 3-5 min or 20mg pushes every 1-2 mins PRN.
Pros: Short-acting sedative/amnestic, easy to redose, near immediate effect, decreased muscle tone for orthopedic procedures.
Cons: No analgesia, has pain on injection, can cause hypotension and respiratory depression.
Special notes:
Use a larger vein, such as in the antecubital fossa.
Recommended to pretreat with opioid (fentanyl, typically 50-100mcg) or ketamine for procedural pain. The downside of opioid pretreatment is greater risk of respiratory depression.
Injection pain can be reduced with intravenous 1% lidocaine mixed with propofol or prior to injecting propofol while occluding the vein. The dose is of lidocaine is 0.5mg/kg or approximately 3-4cc of 1% lidocaine.
Reduce the mg/kg dose in elderly and use lean body weight (calculator) in obese patients. No change is required in patients with impaired liver or kidney function.
Ketamine:
Onset/Duration: Onset of 30 seconds to 1 minute when given IV, duration of 10-20 min.
Dose: When used alone, dose is 1-2mg/kg given over 1-2 min followed by 0.5 mg/kg doses every 5-10 min PRN.
Pros: Dissociative sedative/analgesic with minimal respiratory depression, no impairment of protective airway reflexes, and no hypotension.
Cons: Ketamine can cause emergence reactions or post-sedation agitation (up to 20%), laryngospasm, nausea/vomiting, hypersalivation, tachycardia, and may increase ICP/IOP.
Special Notes:
Midazolam 0.05 mg/kg (2-4mg typically) immediately prior to ketamine can reduce rates of emergence reactions although increases rates of respiratory depression.
Avoid in patients with psychotic disorders.
Recommended for patients who may have a potentially difficult airway because there is less risk for respiratory depression.
This is the first-line medication for children above 3 months of its impeccable airway safety and provides both sedation and analgesia as a single agent (no need for opioids).
Combined Ketamine and Propofol, AKA “Ketofol”:
Onset/Duration: Same as above for each medication.
Dose: 0.5 mg/kg of each medication followed by propofol 0.5 mg/kg doses every 3-5 min or 20 mg pushes every 1-2 mins prn. Of note, individual provider choice of dose for each medication varies widely.
Pros: Potential benefit is ability to use lower doses of both ketamine and propofol with potentially lower risk of adverse events such as hypotension, respiratory depression, emesis, emergence reactions.
Cons: May reduce side effects of each medication individually, yet now dealing with the side effects of two medications rather than one alone.
Special notes:
Research on ketofol is mixed. Systematic reviews have shown that it causes fewer events of respiratory depression and hypotension/bradycardia, yet these events were mostly transient and clinically insignificant. Overall, ketofol has not been shown to reduce clinically significant adverse events or to prolong procedural duration.
Etomidate:
Onset/Duration: Near immediate onset when given IV, duration of 5-15 min.
Dose: 0.1-0.15 mg/kg given over 30-60 seconds, redose every 3-5 min.
Pros: Easy to dose, minimal hemodynamic effect.
Cons: No analgesia, myoclonus (up to 80%), respiratory depression (10%), nausea/vomiting, pain with injection, and potential for adrenal insufficiency.
Special Notes:
Recommended to pretreat with opioid (fentanyl, typically 50-100mcg) for procedural pain. The downside of opioid pretreatment is greater risk of respiratory depression.
In rare cases of severe myoclonus, treat with 1-2 mg IV midazolam every minute until resolved. Some providers pretreat with 0.015 mg/kg etomidate to prevent myoclonus.
Dose must be reduced for patients who are elderly or have renal/hepatic dysfunction.
Not recommended for orthopedic procedures given the frequency of myoclonus.
Midazolam (requires opioid co-administration):
Onset/Duration: Onset of 2-5 min, duration of 30-60 min.
Dose: 0.02-0.03 mg/kg or 0.5-1 mg doses IV every 2-5 min prn, typically not exceeding 5 mg total.
Pros: Provides anxiolysis and amnesia.
Cons: Not as effective for true procedural sedation as shorter acting medications, no analgesia, higher risk of respiratory depression when combined with fentanyl compared to other medications.
Special Notes:
When combining with fentanyl for pain/sedation, give midazolam doses as above first until the desired anxiolysis is achieved, typically 1-2 doses, then give 0.5 mcg/kg doses of fentanyl every 2 min PRN, carefully titrated to effect, with maximum dose of 5 mcg/kg or approximately 250 mcg.
Prolonged sedation is high risk in patients who are elderly, obese, or have hepatic/renal dysfunction.
Use for anxiolysis rather than for true procedural sedation.
Barbiturates (Methohexital):
Onset/Duration: Immediate onset, duration of < 10 min.
Dose: 0.75-1 mg/kg followed by 0.5 mg/kg doses IV every 2 min prn.
Pros: Fast onset, short duration sedation.
Cons: No analgesia, causes hypotension/tachycardia, can precipitate seizures.
Special Notes:
You are probably never going to use this drug unless you are in a very resource limited setting, but you might as well know it is an option.
Dexmedetomidine:
Onset/Duration: Onset of 5-10 min, duration of 60-120 min.
Dose: Not well studied for procedural sedation, options are intranasal 2-3 mcg/kg or bolus of 0.5-1.0 mcg/kg over 10 min followed by infusion of 0.2-0.7 mcg/kg/hr.
Pros: Preserved muscle tone and respiration, much like natural sleep, provides some analgesia.
Cons: Potentially unpredictable effect, not well studied, risk of hypotension/bradycardia, longer acting.
Special Notes:
Delayed time to onset may limit application in the ED
Dexmedetomidine is just not ready for primetime yet, but worth further investigation.
Nitrous oxide:
Onset/Duration: Immediate onset, off within seconds.
Dose: 30-50% mixture with 30% oxygen.
Pros: Provides analgesia, anxiolysis, and sedation all in one.
Cons: Not typically available in emergency departments, needs scavenging system.
Special Notes:
Have been trying for years to get this constantly vented into all our patient rooms, but still no luck with our administration.
Summary Points:
Propofol, ketamine, ketofol, and etomidate are our typical first-line medications in the emergency department for procedural sedation.
Ketamine is preferred for kids.
In adults, propofol or ketofol is best for hemodynamically stable adults requiring procedural sedation, particularly for joint reductions because it does not cause myoclonus and is easy to titrate.
Etomidate provides greater hemodynamic stability and is best for cardioversion or procedures in patients with hemodynamic compromise, but the downside is myoclonus which may reduce procedural success.
Ketamine alone is best in patients with a difficult airway or at high risk for respiratory compromise because it does not cause respiratory depression.
Use what you are most comfortable with, and remember that adequate preparation is key.
Expert Commentary
Thank you for the excellent and concise review. It’s been interesting to see procedural sedation practices change over the course of my training and career, as newer safe and easy options (propofol and ketamine) gained rapid popularity but have been challenged by drug shortages and well-publicized celebrity tragedies. Here is my typical practice, which is certainly not the only correct way but my strong preference:
A few factors on when to think about procedural sedation:
-Any painful procedure, particularly for potential for longer duration. This includes incision and drainage (especially Bartholin’s) and disimpaction. I’ve gotten some odd looks for suggesting it but it works out better for everyone involved.
-Consultant’s procedures, particularly big traumatic injuries which look nasty and like they need to be fixed. It’s easy to forget how terrible it is for the patient.
When I think about avoiding:
-medically complex patients
-difficult airways
-procedures that can wait
-procedures with low likelihood of success even under the best circumstances. If they need to go to the OR no matter what, that might be the best place to start.
My one exception are situations that are currently painful and need to be fixed now and can be fixed quickly, e.g. dislocated ankles. The likelihood of success with 100mcg of fentanyl within seconds to resolve a huge amount of pain now is exceedingly favorable.
The worst situation is trying to avoid procedural sedation with “just some morphine and maybe a little lorazepam” which quickly devolves into “a little more morphine” and “hmm maybe another dose of lorazepam.” Now it’s a procedural sedation that is both ineffective and unsafe.
My general process:
First I print out a checklist I made with the following preparation steps (details below):
RSI box (succinylcholine)
VL
airway cart (LMA, PEEP valve, DL gear)
nasal ETCO2 (plus ETT adapter)
4mg ondansetron now
bottle ketamine
bottle propofol
room ready (including suction, bag, anything required for the procedure)
Department ready?
Am I ready?
Procedure plan
Post-procedure planning (sling, splint)
The general principle is to set up at least as much as if I were performing RSI. A lot of this may seem like over-preparation, but the more I prepare, the luckier I get. Here is some more detail on each item:
RSI box (succinylcholine)
2 main purposes for the RSI box. First, if things go south, I will be intubating the patient, and need the medications to do so (i.e. NMBA). Second, if I am using ketamine, there is a small but nontrivial chance of laryngospasm, and of jaw thrust and bagging do not fix it, the patient needs NMBA. This is not a time to debate roc vs sux, so I always have sux in the room (even if roc isn’t slower when dosed appropriately at ≥1.2mg/kg, I don’t want to have to argue about it at the RCA). The easiest way for me to get these medications in the room is grabbing our RSI box, but this will depend on your department; simply grabbing a vial of sux with 1.5mg/kg is sufficient.
VL
If things go south, this is not the time for the intern to practice their DL. I always have the hyperangulated VL ready to go at the head of the bed, with a combo Mac VL/DL blade and a traditional Mac DL as backup, with stylets loaded with tubes ready to go.
Airway cart
We have nicely built airway carts with everything I need for bagging, difficult bagging, and difficult intubation. Primarily, what I want is gear for bagging, i.e. LMA and PEEP valve. All the usual backup is here as well (oral/nasal airways, bougie, cric gear).
Nasal ETCO2 (and ETT adapter)
The literature on end tidal in procedural sedation is interesting but I think generally answers a different question than the one I care about. I don’t look for qualitative changes in waveforms or quantitative changes in ETCO2 to predict hypoventilation; rather, it is the quickest and easiest way to see if the patient is breathing. No staring at their chest hoping to see chest rise. Simply look at the monitor: either there is a waveform and they are breathing, or there is not and they are not. It’s like a sedative for me, similar to supervising an intern using VL instead of DL: it makes the procedure much less stressful for me.
Additionally, by using ETCO2, it is now safe to provide supplemental oxygen via nasal cannula or reservoir facemask so if things go south, there is a much wider safety margin (i.e. the patient is preoxygenated for intubation).
4mg ondansetron now
As discussed above, it might help, it may not, and it’s safe and easy.
bottle Ketamine
bottle Propofol
I’ll discuss my medication strategies below, but the bottom line is I like to have multiple 100s of mg of each medication ready for each patient, because when I need to redose, it can be needed in a very short time.
Room ready
Other equipment I make sure is ready: suction, bag for mask ventilation. Other items like do I need vaseline gauze for splinting over an abrasion?
Is the Department ready?
Was an 80 year old with abdominal pain just roomed? Should I lay eyes on them and make a quick decision about an obvious CT? Is there a hospitalist hanging around who I can tell about another patient to send upstairs before I get stuck in a sedation for 45 minutes? Should I discharge anyone?
Am I ready?
Do I need to go to the bathroom? Has it been hours before I’ve had any calories?
Procedure plan
I always make sure to have a clear plan for the procedure—not just the sedation—well before we start. Who is doing what? What technique are we using? What are backup plans? Of course these questions apply to the sedation as well.
If a non-EM physicians is performing the procedure (e.g. ortho, or gen surg pulling a tunneled line) I try to make sure that they understand my definition of “ready” is not the same as in the OR, and I make sure they are ready to start the actual procedure as soon as the meds are working. This is not a judgment in any way; rather, the ER simply isn’t the OR.
Post-procedure planning
Few things are more frustrating than getting a difficult shoulder reduced only to have it slip out while someone is hunting down the sling I forget to get beforehand, that I knew I would need (see also: ordering post-intubation meds with RSI meds in an intubation). Obviously if something needs to be splinted we need the gear and whoever is doing the splint. And, if there are abrasions going under the splint, petroleum gauze, etc.
Medication choices
I typically choose between ketamine and propofol on a spectrum.
Factors on the propofol side: young, healthy, BP/respiratory reserve, shorter procedure, ortho procedure (propofol is much better at loosening up patients, plus these often end quickly).
Factors on the ketamine side: older, more comorbidities, less respiratory reserve, longer procedures, non-reduction procedures, more protractedly-painful procedures (e.g. I&D).
Obviously these are not absolutes and I tend to plan on using ketofol quite a bit. I usually have enough cognitive space and hands available to dose them separately (generally 0.5mg/kg ketamine first, then 0.5mg/kg propofol as needed) but in more constricted settings I will mix 1:1 if I don’t have the bandwidth.
I will say I have been tending to more and more ketamine-only sedations. Usually I start with the intention of using ketamine-first ketofol, particularly if the patient needs to be loosened up for a reduction, but I am continually surprised by how little I end up needing the propofol.
As noted above, for solo propofol, I pretreat with fentanyl as propofol is not inherently analgesic.
I appreciate the debate about midazolam for pretreatment for ketamine, but the rates of substantial post-sedation agitation are low enough that I simply treat that when it happens, as not all but most ketamine respiratory depression only happens with co-administered sedatives.
Other than lack of availability of other options, there is no reason to use fentanyl/midaz anymore.
Lastly, I’ve stopped using etomidate. The rate of myoclonus is simply too high. Myoclonus easily defeats the reduction, and even for cardioversion, it makes checking the rhythm, getting an ECG, monitoring the sat, etc. very difficult. Ultimately, it’s just a headache we don’t need, particularly as we have so many other safe and effective agents.
As I said above, these are more my style preferences than the only absolutely correct choices, and I am always happy to at least discuss adapt to the circumstances including others’ preferences (or trying something different so the residents can gain experience with different techniques).
Seth Trueger, MD, MPH, FACEP
Assistant Professor
Northwestern Emergency Medicine
Citations
Brown TB, Lovato LM, Parker D. Procedural sedation in the acute care setting. Am Fam Physician 2005; 71:85.
Swanson ER, Seaberg DC, Mathias S. The use of propofol for sedation in the emergency department. Acad Emerg Med 1996; 3:234.
Miner JR, Burton JH. Clinical practice advisory: Emergency department procedural sedation with propofol. Ann Emerg Med 2007; 50:182.
Euasobhon P, Dej‐arkom S, Siriussawakul A, Muangman S, Sriraj W, Pattanittum P, Lumbiganon P. Lidocaine for reducing propofol‐induced pain on induction of anaesthesia in adults. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD007874. DOI: 10.1002/14651858.CD007874.pub2.
Messenger DW, Murray HE, Dungey PE, et al. Subdissociative-dose ketamine versus fentanyl for analgesia during propofol procedural sedation: a randomized clinical trial. Acad Emerg Med 2008; 15:877.
Strayer RJ, Nelson LS. Adverse events associated with ketamine for procedural sedation in adults. Am J Emerg Med 2008; 26:985.
Adnolfatto G et al. Ketamine-Propofol Combination (Ketofol) versus propofol alone for Emergency Department Procedural Sedation and Analgesia: A Randomized Double-Blind Trial. Annals of Emergency Medicine. 2012;59(6):504-512.e2
Miner JR et al. Randomized, Double-Blinded, Clinical Trial of Propofol, 1:1 Propofol/Ketamine, and 4:1 Propofol/Ketamine for Deep Procedural Sedation in the Emergency Department. Annals of Emergency Medicine. 2015;65(5):479-488.e2
Yan JW, McLeod SL, Iansavitchene A. Ketamine-Propofol Versus Propofol Alone for Procedural Sedation in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emerg Med 2015; 22:1003.
Miner JR, Danahy M, Moch A, Biros M. Randomized clinical trial of etomidate versus propofol for procedural sedation in the emergency department. Ann Emerg Med 2007; 49:15.
Falk J, Zed PJ. Etomidate for procedural sedation in the emergency department. Ann Pharmacother 2004; 38:1272.
Sacchetti A, Senula G, Strickland J, Dubin R. Procedural sedation in the community emergency department: initial results of the ProSCED registry. Acad Emerg Med 2007; 14:41.
Keim SM, Erstad BL, Sakles JC, Davis V. Etomidate for procedural sedation in the emergency department. Pharmacotherapy 2002; 22:586.
Hüter L, Schreiber T, Gugel M, Schwarzkopf K. Low-dose intravenous midazolam reduces etomidate-induced myoclonus: a prospective, randomized study in patients undergoing elective cardioversion. Anesth Analg 2007; 105:1298.
Horn E, Nesbit SA. Pharmacology and pharmacokinetics of sedatives and analgesics. Gastrointest Endosc Clin N Am 2004; 14:247.
Bahn EL, Holt KR. Procedural sedation and analgesia: a review and new concepts. Emerg Med Clin North Am 2005; 23:503.
Frank RL. Procedural sedation in adults outside the operating room. Wolfson AB, and Grayzel J (Ed.) UpToDate (2018).
Hsu DC and Cravero JP Pharmacologic agents for pediatric procedural sedation outside of the operating room. Stack AM and Randolph AG (Ed.) UpToDate (2018).
G. Haeseler, M. Störmer, J. Bufler, R. Dengler, H. Hecker, S. Piepenbrock, et al. Propofol blocks human skeletal muscle sodium channels in a voltage-dependent manner. Anesth Analg, 92 (2001), pp. 1192-1198
J. Ingrande, H. J. M. Lemmens; Dose adjustment of anaesthetics in the morbidly obese, BJA: British Journal of Anaesthesia, Volume 105, Issue suppl_1, 1 December 2010, Pages i16–i23.
Neuman G and Koren G. Safety of Procedural Sedation in Pregnancy. J Obstet Gynaecol Can. February 2013, pages 168-173.
How To Cite This Post
[Peer-Reviewed, Web Publication] Conrardy M, LaPlant W. (2019, Nov 11). Procedural Sedation. [NUEM Blog. Expert Commentary by Trueger S]. Retrieved from http://www.nuemblog.com/blog/procedural-sedation.
Ultrasound Confirmation of Endotracheal Tube Placement
Written by: Maurice Hajjar, MD (NUEM PGY-2) Edited by: Alex Ireland, MD (NUEM PGY-4) Expert commentary by: John Bailitz, MD
Introduction
Although the cuff is inflated and the laryngoscope is removed, no emergent intubation is complete without first confirming the correct placement of the endotracheal tube (ETT). A variety of indicators exist that can confirm ETT placement into the trachea rather than the esophagus—chest rise, condensation in the tube, auscultation of breath sounds, lack of abdominal breath sounds, visualization with a video or fiberoptic laryngoscope, and both quantitative waveform capnography and qualitative (or colorimetric) capnometry.
However, situations exist in which these techniques may be unavailable, impractical, or can even fail or mislead providers. A hectic cardiac arrest scenario may present the perfect storm. Chest compressions preclude providers from visualizing chest rise. Gastric contents or blood can mask tube condensation or preclude visualization of the cords with a video laryngoscope. Colorimetric capnometry can have low sensitivity in patients without a palpable pulse and can also be falsely positive if exposed to blood or gastric contents [1]. The sensitivity of quantitative waveform capnography decreases significantly in cardiac arrest as it requires adequate pulmonary circulation which may be absent in this or other low flow states [2,3]. Furthermore, despite increasing use, it may be unavailable at the institution altogether [4].
Taken together, there is a relatively high risk of esophageal intubation in this scenario which bears disastrous consequences. Any single method of confirming ETT placement is imperfect; as such, there is room for unique modalities in emergent intubations.
Using Point of Care Ultrasound to Confirm Endotracheal Tube Placement
Why it works
Point of care ultrasound (POCUS) is readily available in emergency departments (EDs) and intensive care units in most settings and both intensivists and emergency providers have at least some training in its use at the bedside. Conceptually, the use of transtracheal US to confirm ETT placement relies on the differing anatomy of the trachea and esophagus. Recall that the trachea remains open due to cartilaginous rings while the esophagus will collapse unless filled (e.g., by an ETT). Thus, an esophagus with an ETT will be more readily visualized adjacent to the trachea than one without.
The sonographic appearance of the trachea is characterized by a bright, hyperechoic curvilinear structure with posterior shadowing and reverberation artifact (Figure 1). If the trachea was intubated, then a single bullet sign [5] (Figure 2) will be visualized, which is an increase in both the echogenicity and the posterior artifact indicating the presence of an air-filled ETT.
Figure 1: Sonographic view of trachea showing air-mucosa interface with posterior reverberation and shadowing artifact. [Photo courtesy of John Bailitz, MD]
Figure 2: Clip demonstrating the bullet sign: a single air-mucosa interface with increased posterior shadowing and artifact indicates the trachea has been intubated. [Photo courtesy of John Bailitz, MD]
Conversely, if the esophagus is intubated, then a double tract sign [6] (Figure 3) will be visualized, which is the appearance of a “second” trachea, or a similar hyperechoic line with posterior shadowing and reverberation artifact lateral to that of the trachea. This second air-mucosa interface indicates that the esophagus is stented open by an air-filled ETT.
Figure 3: Clip demonstrating the double tract sign: the appearance of a second air-mucosa interface with posterior artifact adjacent to the trachea indicates the esophagus has been intubated. [Photo courtesy of John Bailitz, MD]
How it is used
As alluded to above, the primary use of US in confirming ETT placement is determining that the trachea, rather than the esophagus, has been intubated. This can be confirmed either statically or dynamically. In static confirmation, the US probe is used post-intubation to visualize either the bullet sign or the double tract sign. Additionally, if the operator is uncertain, she or he could lightly move the ETT up and down to ascertain if there is movement in the region of the trachea or esophagus7. In dynamic confirmation, the US probe is used during intubation to visualize the increase in artifact as the tube passes into the trachea or the appearance of artifact as the tube passes into the esophagus.
Of note, transtracheal US cannot be used to determine the distance of the ETT from the carina or to determine if the right mainstem bronchus has been intubated. Thoracic ultrasound, however, can be used to observe bilateral pleural sliding but requires multiple ventilations. Additionally, anatomical variance may cause the esophagus to be positioned directly posterior to the trachea, leading to false positive tracheal intubations [8].
Technique [6–8]
Use a high frequency linear probe with sonographic gel applied liberally.
Place the probe superior to the suprasternal notch in a transverse orientation, being careful to minimize downward pressure.
Adjust sonographic depth (depending on body habitus) to visualize the trachea and, if visible, the esophagus which will typically lie posterolateral to the trachea.
Interpret:
If performing static confirmation post-intubation, look for the bullet sign or the double tract sign.
If performing dynamic confirmation during intubation, look for an increase in motion artifact posterior to the trachea or the appearance of a “second” trachea (double tract sign).
Brief Review of Evidence
A meta-analysis pooled data from 11 studies and 969 intubations and showed an aggregate sensitivity of 98% and specificity of 94% in emergency intubations, with capnography as the gold standard [5]. More recently, a meta-analysis of 17 studies and 1,596 patients showed a sensitivity of 98.7% and specificity of 97.1%, with a positive likelihood ratio of 34.4 and a negative likelihood ratio of 0.019. This compares favorably to pooled data from studies examining capnography, which in one meta-analysis showed slightly lower sensitivity but similar specificity (93% and 97%, respectively)2,10. Furthermore, POCUS has several distinct advantages over capnography as mentioned above.
POCUS is a skill familiar to many ED providers. A pilot study in a non-emergent, controlled operating room setting of patients intubated by anesthesiologists demonstrated that ED providers with no formal airway US training could identify tracheal intubations with a sensitivity and specificity approaching 100% [8]. In a cadaver study, the performance of residents compared favorably to that of ultrasound fellowship-trained emergency physicians, ranging from 91-100% sensitivity and 48-96% specificity depending on cadaver body habitus [11].
In the emergent setting, ultrasound assessment not only has high sensitivity and specificity for tracheal intubation but can be performed rapidly. A study of patients being intubated for impending respiratory failure, cardiac arrest, or trauma found that ED residents trained in airway US could identify tracheal intubation using ultrasound with 98.9% sensitivity, 94.1% specificity, and a 93% concordance with criterion standard quantitative capnography. Furthermore, confirmation of ETT tube with ultrasonography could be performed within an average of nine seconds [6]. During CPR, real-time tracheal ultrasonography was 100% sensitive and 85.7% specific for detecting tracheal versus esophageal intubation compared to the combined criterion standard of waveform capnography and auscultation. Furthermore, this study examined ultrasonography performed during chest compressions, suggesting that ultrasonography can be a highly reliable method of ETT confirmation without interrupting compressions [12].
Summary
Established methods of confirming ETT placement in an emergent intubation are imperfect.
Quantitative waveform capnography has reduced sensitivity in the setting of a cardiac arrest or other low-flow states and requires multiple ventilations prior to confirmation.
Ultrasound can rapidly be used to confirm ETT placement with comparable sensitivity and specificity to criterion standards without requiring ventilation or an interruption of chest compressions.
Providers with some familiarity with US can use it to distinguish between tracheal and esophageal intubations reliably.
Expert Commentary
Thank you for his outstanding review of an exciting and relatively new application in Emergency Ultrasound. Although the literature on this topic has exploded in the last few years, tracheal ultrasound was already included in the 2015 ACLS Guidelines as a reliable method to confirm endotracheal intubation.
As a longtime ultrasonographer and resuscitationist, I find this application particularly useful in two common ED situations. The first is out of hospital cardiopulmonary arrest in which the patient was already intubated by paramedics in the field. As the patient arrives in the resuscitation bay, there are a number of competing priorities. Rapid confirmation of correct endotracheal tube placement during chest compressions allows the team to quickly move on to other priorities. The second is the difficult intubation of the crashing ED patient. Particularly, in patients who are obese or otherwise have distorted airway anatomy, the ultrasound machine provides real time visualization of the endotracheal tube placement, or a rapid confirmation immediately after. In either situation, the ultrasound machine will certainly be helpful not only for confirmation of ETT location, but further for ruling out pneumothorax and main stem intubation, before moving onto other causes of cardiac arrest such as cardiac tamponade, massive PE, and blood loss.
Regarding technique, dynamic visualization during intubation may be difficult particularly if external laryngeal manipulation while is being preformed. So static visualization immediately after placement is often more feasible. Forceful, or up and down movement of the tube may dislodge an endotracheal tube, damage the airway, or stimulate a cough or vomiting in the non-paralyzed patient. Instead, simply gently rotating the tube from side to side creates an easily visible change in the tracheal air column if correctly located, or “esophageal sliding” of the mucosa over the endotracheal tube if incorrectly placed in the esophagus.
Final shout outs to the authors of this well written blog. But also to Dr. Michael Gottlieb, full disclosure my former fellow, for his considerable research in this area. Dr. Gottlieb first identified the need for better confirmatory methods as an EM intern. Although I was initially skeptical as a resuscitationist, Dr. Gottlieb quickly convinced me with a well-done literature review during which he identified a gap in the existing literature. Dr. Gottlieb then took the initiative and turned one research question into an exciting are of scholarship for his career and the many fellows that followed that benefitted from Dr. Gottlieb’s mentoring. This is such a wonderful example of turning a simple clinical question into a rich and rewarding area of leadership through scholarship!
John Bailitz, MD
Vice Chair for Academics
Department of Emergency Medicine
Northwestern Feinberg School of Medicine
Citations
1. MacLeod BA, Heller MB, Gerard J, Yealy DM, Menegazzi JJ. Verification of endotracheal tube placement with colorimetric end-tidal CO2 detection. Ann Emerg Med [Internet] 1991 [cited 2019 Jan 8];20(3):267–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1899985
2. Li J. Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation. J Emerg Med [Internet] 2001 [cited 2019 Jan 8];20(3):223–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11267809
3. Takeda T, Tanigawa K, Tanaka H, Hayashi Y, Goto E, Tanaka K. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation [Internet] 2003 [cited 2019 Jan 8];56(2):153–7. Available from: https://www.sciencedirect.com/science/article/pii/S0300957202003453
4. DeIorio NM. Continuous end-tidal carbon dioxide monitoring for confirmation of endotracheal tube placement is neither widely available nor consistently applied by emergency physicians. Emerg Med J [Internet] 2005 [cited 2019 Jan 13];22(7):490–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15983084
5. Das SK, Choupoo NS, Haldar R, Lahkar A. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anesth Can d’anesthésie [Internet] 2015 [cited 2019 Jan 11];62(4):413–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25537734
6. Chou H-C, Tseng W-P, Wang C-H, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation [Internet] 2011 [cited 2019 Jan 9];82(10):1279–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21684668
7. Chao A, Gharahbaghian L. Tips and Tricks: Airway Ultrasound [Internet]. Am. Coll. Emerg. Physicians Emerg. Ultrasound Sect. 2015 [cited 2019 Jan 13];Available from: https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/june-2015/tips-and-tricks-airway-ultrasound/#sm.00000hnz0e2u2ofnizwz7io2f5wg6
8. Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med [Internet] 2007 [cited 2019 Jan 9];49(1):75–80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17014927
9. Gottlieb M, Holladay D, Peksa GD. Ultrasonography for the Confirmation of Endotracheal Tube Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med [Internet] 2018 [cited 2019 Jan 16];72(6):627–36. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30119943
10. Gottlieb M, Bailitz J. Can Transtracheal Ultrasonography Be Used to Verify Endotracheal Tube Placement? Ann Emerg Med [Internet] 2015 [cited 2019 Jan 11];66(4):394–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25805115
11. Gottlieb M, Bailitz JM, Christian E, et al. Accuracy of a novel ultrasound technique for confirmation of endotracheal intubation by expert and novice emergency physicians. West J Emerg Med [Internet] 2014 [cited 2019 Jan 13];15(7):834–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25493129
12. Chou H-C, Chong K-M, Sim S-S, et al. Real-time tracheal ultrasonography for confirmation of endotracheal tube placement during cardiopulmonary resuscitation. Resuscitation [Internet] 2013 [cited 2019 Jan 10];84(12):1708–12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23851048
How To Cite This Post
[Peer-Reviewed, Web Publication] Hajjar M, Ireland A. (2019, Nov 4). Ultrasound Confirmation of ETT Placement. [NUEM Blog. Expert Commentary by Bailitz J]. Retrieved from http://www.nuemblog.com/blog/us-ett.
Other Posts You May Enjoy
Needlestick Injuries
Written by: Logan Wedel, MD (NUEM PGY-2) Edited by: Hashim Zaidi, MD (NUEM ‘19) Expert commentary by: Tim Loftus, MD, MBA
So You Just Sustained A Needlestick Injury… Now What?
A Brief Guide For Healthcare Professionals
Needlestick injuries continue to be a common source of work related injury among health care professionals.
Since the Needle-Stick Safety and Prevent act of 2000, non-surgical needle sticks have decreased by 31.6% (2001-2006). Over this same time period, incidents within the surgical setting have increased 6.5%.
However the most recent data from the CDC still estimates 385,000 injuries a year, which equates to more than 1,000 needle stick injuries per day amongst health care professionals. Unfortunately, this is believed to be a gross under-estimation secondary to the vast amount of incidents that go un-reported.
So I Got Stuck… What Is My Actual Risk?
High Risk
Inoculation from deep or open wound
Stick with a hallow bore needle / Needle used for blood draw
Low Risk
Suturing needle
Discarded needle
No Risk
Unused needle
No break in the skin
Good News! The risk of occupational transmission is low!
Transmission Rates by Disease - From a Source Positive Patient
Hepatitis B: 1% - 62% (Depending on exposure type and infectivity of source patient)
Risk of developing clinical evidence of infection ranges from 1% - 31%
Risk of developing serologic evidence of infection ranges from 23% - 62%
Fortunately, this disease is the most easily prevented. Staying up to date on vaccines is the #1 way to prevent HBV infection!
Hepatitis C: 1.8%
Has ranged from 0% - 7% in some studies
Extremely low transmission rates from mucous membrane exposure
Human Immunodeficiency Virus (HIV): 0.3%
Rates drop to 0.09% with mucous membrane exposure
Immediately After Exposure
Safely cease the procedure. Have another operator take over if available.
The best way to prevent transmission after contact is to wash the site thoroughly with soap and water
Take your time to perform this well
Flush the nose and mouth if they were exposed
Copious irrigation of the eyes if there was ocular exposure
Reporting
This is the last thing you want to be doing, but....
It is critical to report the incident. Each institution has its own protocol that health care professionals are required to follow. The first step usually deals with informing the charge nurse or unit manager if you are in a healthcare facility. Follow your local institutional protocols to document and report the exposure.
Every healthcare facility has protocols for occupational exposure. Remember-this is not a unique event and these exposures happen. If there is uncertainty on how to proceed, see if the institution has infection control personnel, occupational health agents, or other administrators or staff who would be familiar with the process.
This happens. Follow the institutional process and remember this is not uncommon. By not reporting or following protocol you risk transmission of blood borne infectious agents without timely diagnosis and treatment.
Management + Blood Draws
1. Collect the Source Patient's Blood -- Disclose the Incident
If unable to acquire (patient no longer present, refuses, or unknown source), post-exposure prophylaxis will need to be considered carefully
Council the source patient on the standard practice to test for blood born infectious agents given the exposure
Determine the source patient's baseline disease characteristics and any treatment history
2. Your Blood Work
Determine your baseline disease characteristics
Hepatitis B status
Vaccinated with or without response
Un-vaccinated without infection
Evidence of current infectivity
Hepatitis B immune globulin (HBIG) may be utilized post exposure particularly for those who are not vaccinated
Hepatitis C status
HIV status
3. Follow Up Blood Work - Short and Long Term Monitoring
Hepatitis B: repeat test at 6 months post exposure
Hepatitis C: repeat testing at 2, 4, 8 weeks post exposure
HIV : repeat testing at 6 weeks, 3 months, 6 months, 1 year post exposure
Post Exposure Prophylaxis
Hepatitis B
Hepatitis B Immune Globulin Alongside Vaccination Series
Roughly 75% effective and preventing infection
Administer ASAP - effectiveness after 7 days is unclear
Hepatitis C
No available post exposure prophylaxis
Follow your blood work to monitor disease status
Human Immunodeficiency Virus (HIV):
Three Drug Cocktail: Truvada QD (Tenofovir 300mg + Emtricitabine 200mg) + Raltegravir 400mg BID is the preferred regimen
Dual Nucleoside Reverse Transcriptase Inhibitor +
Integrase Inhibitor
Protease Inhibitor
Non Nucleoside Reverse Transcriptase Inhibitor
Multiple Regimens Exist: Can target specific resistance patterns. Expert consultation can be made with local experts or by calling the National Clinicians’ Post-Exposure Prophylaxis Hotline (PEPline) at 888-448-4911.
Initiate ASAP - effectiveness unknown after 72 hours
28 Day Regimen
Close physician/laboratory follow up to monitor toxicity
Prevention
Always take the the time to apply proper personal protective equipment (PPE)
It will save you time and save you stress
Gowns, Gloves, Goggles
Common mistake to forget eye protection
Double glove in higher risk circumstances
Safe practices: Never reuse needle / Never re-cap needle
Safe needle disposal
Expert Commentary
Thank you to Dr. Wedel on an excellent review and summation of what is a frequent and yet frustrating topic for EM physicians. The evaluation and management of potential blood or body fluid exposures is an area riddled with logistical nuances that frequently change and can be state and institution-specific. As such, it can be very helpful to mentally break the topic down as has been done so nicely here, into considerations of risk, reporting, testing, and management (including PEP). There are a few important points and nuances that deserve further discussion:
Safety
Safety is of utmost priority - safety for yourself, your colleagues, and your patients and their family members. These events are vastly underreported for a variety of reasons, but often this is the first step in tracking these events, mitigating downstream morbidity, addressing issues upfront, and preventing transmission. A safety culture is built on a daily basis by each and every one of us.
Nature of Exposure
This post focuses on occupational exposures to healthcare workers, which are relevant to us, but are by far not the only possible or definite exposure we will see. The more detailed and thorough history we can elicit in these situations may make the difference between initiation or not of post-exposure prophylaxis, as an example. It is incumbent upon us in emergency medicine to remain up to date on state and local laws and regulations as well as institutional policies and procedures, which help guide us to correctly managing these situations. As an example, the evaluation and management plan of an exposed healthcare worker may differ compared to that of a patient’s family member, pregnant female, or law enforcement officer or other government official. The more details we can gather regarding the nature of exposure and possible risk of blood-borne pathogen transmission will help us in these nuanced situations.
Post-Exposure Prophylaxis
This is nicely outlined by Dr. Wedel - to highlight a few points:
HBV - immunization is key. Please ensure your own HBV immunization status is up to date and obtain history of HBV immunization in all patients who are able to provide this.
Tetanus - depending on the nature of the exposure, be mindful that tetanus immunization may be necessary.
HIV - post-exposure prophylaxis has been shown to be very effective in this situation, decreasing likelihood of HIV transmission by as much as 81%. The effectiveness is best the sooner it gets started after the exposure and is recommended within 72 hours. While there are widely used and preferred regimens, the specific details of each situation may alter the choice of PEP regimen, including kidney function, source patient’s HIV status and resistance patterns, pregnancy, cost, dosing frequency, and side effect profile. The decision to initiate PEP should be involve a detailed and informed conversation with the patient, as 50% of HCW’s have reported side effects to PEP and as many as 33% have prematurely stopping taking the medicines.
Consent
Make sure to consider one’s local practice environment, policies, and procedures with respect to potential body fluid exposure testing and treatment. Certain states, such as Illinois, require consent, pre-test information, and other considerations when performing HIV testing in the ED setting. However, as is the case in Illinois with the AIDS Confidentiality Act and in as many as 35 other states, informed consent and pre-test information may not be required when HIV testing is either medically indicated or in cases of blood or body fluid exposure with certain individuals, including health care workers, law enforcement officers, and paramedics. Be mindful that exception from informed consent does not compel the source patient to submit to testing if a blood specimen is not already available, as this usually requires a court order. Further, exception from informed consent does not waive us of the responsibility to thoroughly discuss with these patients the rationale behind testing, reporting, and details of unconsented HIV testing.
Overall, blood and body fluid exposure in the health care setting is extremely common and relatively easy to manage, but often gets relegated to standard institutional protocols that may or may not be applied appropriately given the unique circumstances of each patient encounter. Thank you again to Dr. Wedel for an excellent review, as a thoughtful approach to these situations can help guide us in having a detailed, informed conversation with our patients surrounding transmission risk, testing procedures, post exposure prophylaxis, and rationale behind follow-up timing and testing procedures.
There are many resources out there to help us, including each institution’s corporate/occupational health, risk management, state and local laws and regulations, and the PEPline.
AIDS Confidentiality Act (410 ILCS 305): http://www.ilga.gov/legislation/ilcs/ilcs3.asp?ActID=1550&ChapterID=35
Cowan E & Macklin R. Unconsented HIV Testing in Cases of Occupational Exposure - Ethics, Law, and Policy. Acad Emerg Med. 2012. 19(10):1181-1187. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3473147/pdf/nihms-402780.pdf doi:10.1111/j.1553-2712.2012.01453.x.
ACEP Policy Statement: https://www.acep.org/patient-care/policy-statements/bloodborne-pathogens-in-emergency-medicine/
Timothy Loftus, MD, MBA
Assistant Professor
Department of Emergency Medicine
Northwestern University
How to Cite this Post
[Peer-Reviewed, Web Publication] Wedel L, Zaidi H. (2019, Oct 14). Needlestick Injuries. [NUEM Blog. Expert Commentary by Loftus T]. Retrieved from http://www.nuemblog.com/blog/needlestick.
Other Posts You Might Enjoy…
References
"CDC Guidance for Evaluating Health-Care Personnel for Hepatitis B Virus Protection and for Administering Postexposure Prophylaxis Management." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/mmwr/PDF/rr/rr6210.pdf.
"Exposure to Blood: What Healthcare Personnel Need to Know." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/HAI/pdfs/bbp/Exp_to_Blood.pdf.
"HIV/AIDS PEP." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/hiv/basics/pep.html.
"HIV/AIDS Post Exposure Prophylaxis (PEP)." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/hiv/risk/pep/index.html
"Oral Health: Occupational Exposure to Blood." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/oralhealth/infectioncontrol/questions/occupational-exposure.html.
"The National Surveillance System for Healthcare Workers." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/nhsn/PDFs/NaSH/NaSH-Report-6-2011.pdf
"Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis." Centers for Disease Control and Prevention, U.S. Department of Health & Human Services, https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5011a1.htm.
The Use of the Angiocatheter in Central Venous Line Insertion
There are two techniques for guide wire insertion when performing central line placement. This week we compare the evidence for the two approaches and provide support for the cathether-over-needle (CON) technique which may prove useful in specific situations.
Quick Guide To Minor Facial Trauma: Part 2
In the emergency department, we commonly encounter minor injuries to the face and mouth. In a two part series, we will provide a short overview of some helpful strategies for dealing with these cosmetically sensitive injuries in an effective manner.
Perimortem Procedures: Yes or No?
We delve into the heated topic of perimortem procedures specifically concerning the ethics, legality, and repercussions of performing procedures on the recently deceased.
Owning The Ankle Arthrocentesis
As ER doctors, we stick a lot of needles into a lot of different body parts. Sometimes into vessels, sometimes into the area around the spinal cord, and of course, sometimes into hot, swollen joints. The ankle is included in this which can often prove difficult to access. To help you through your next angry ankle, here are a couple of pointers.
The Best Agent For Digital Nerve Blocks
Explore the evidence behind previously held beliefs regarding local anesthetic use in digital nerve blocks.
Complications of Central Venous Catheters
We review the recent randomized-controlled trial by Parienti et al in the New England Journal of Medicine which sought to determine the complication rate of central venous catheters (CVC) at the 3 primary sites of insertion.
Wet, Wacky Lungs: A Quick Look At Pleural Effusions
According to the National Cancer Institute, there are 100,000 pleural effusions diagnosed every year. Read on to optimize your management of this very common ED presentation and know whether or not you should "tap that."

























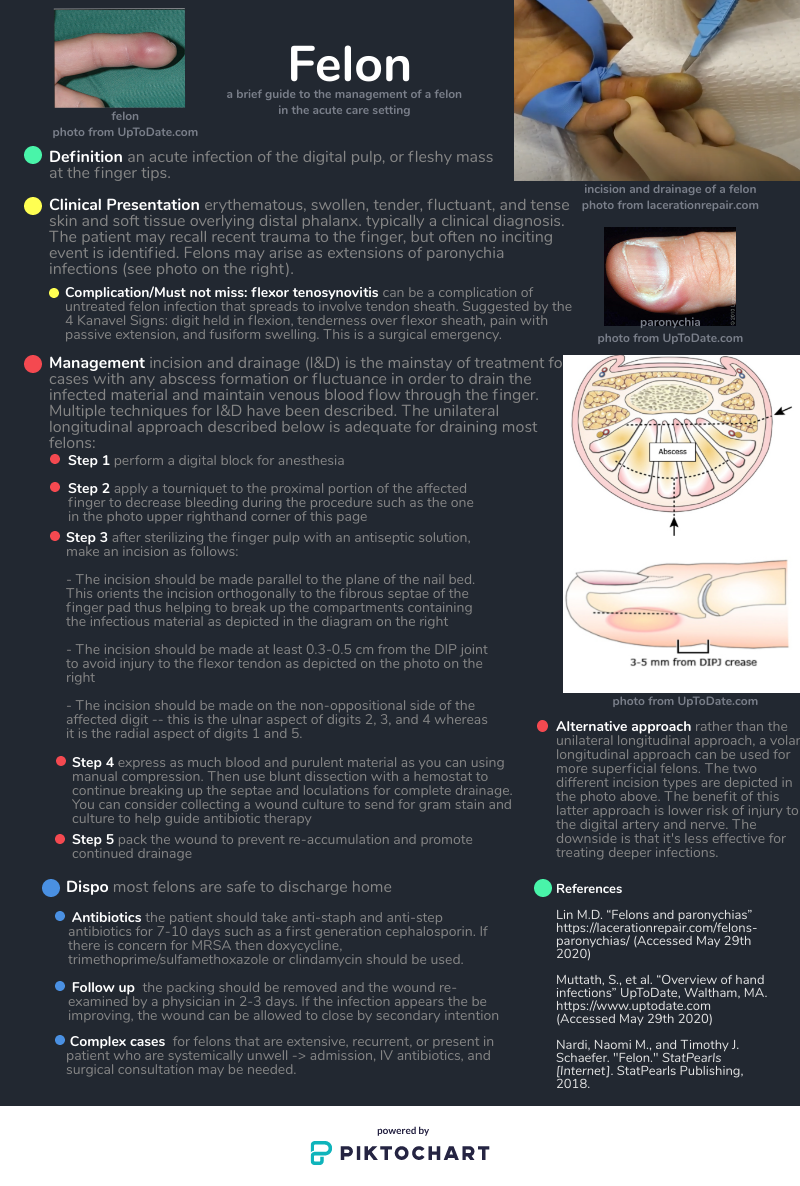











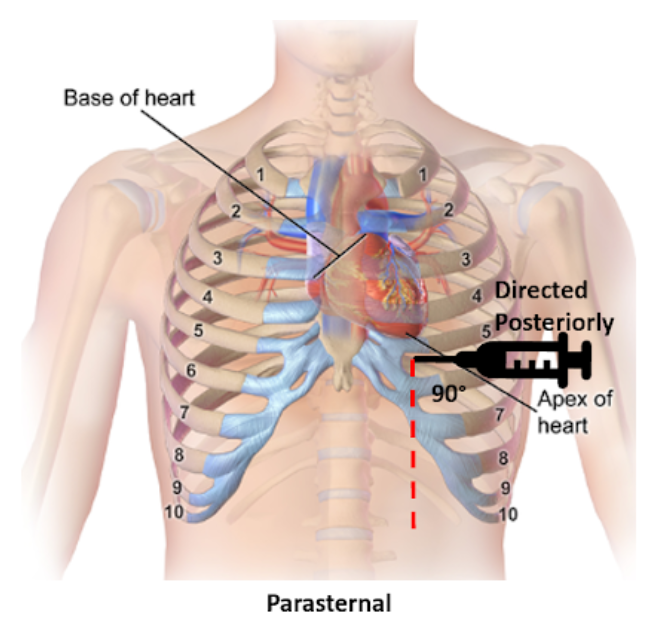























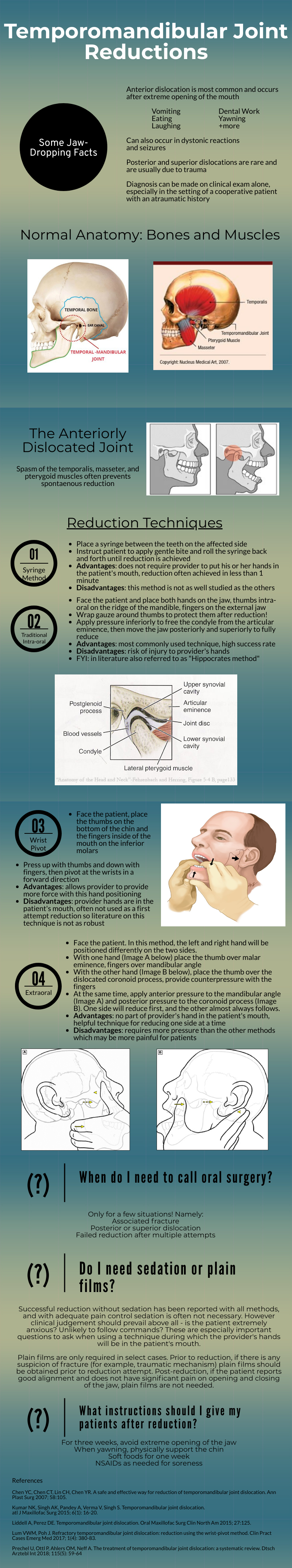













![Figure 1: Sonographic view of trachea showing air-mucosa interface with posterior reverberation and shadowing artifact. [Photo courtesy of John Bailitz, MD]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1572626234251-VL5QSV3R6S608OO7J8OI/1.+Figure+1+-+Trachea.png)
![Figure 2: Clip demonstrating the bullet sign: a single air-mucosa interface with increased posterior shadowing and artifact indicates the trachea has been intubated. [Photo courtesy of John Bailitz, MD]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1572626261525-86AN0IKGCSGN5EHY11VN/image-asset.gif)
![Figure 3: Clip demonstrating the double tract sign: the appearance of a second air-mucosa interface with posterior artifact adjacent to the trachea indicates the esophagus has been intubated. [Photo courtesy of John Bailitz, MD]](https://images.squarespace-cdn.com/content/v1/549b0d5fe4b031a76584e558/1572626372841-E4OFNNGZHEOI7ECDRIJP/3.+Figure+3+-+Double+Tract+Sign.gif)


