Written by: Andra Farcas, MD (PGY-3) Edited by: Jessica Bode, MD (NUEM ‘19) Expert Commentary by: Matthew Levine, MD
Clinical Question:
Are we impeding our patients’ fracture healing by giving them NSAIDs?
Why is this important?
Broken bones hurt. A lot. And we want to do something about that to make our patients feel better. In the context of the current opioid crisis and the controversy of prescribing opioids, we need good non-opioid alternatives. Enter NSAIDs. Multiple studies have investigated whether nonsteroidal anti-inflammatory drugs (NSAIDs) are efficient pain relievers in multiple scenarios, including fractures, and the consensus seems to lean towards yes. However, this is not a discussion about their effectiveness but rather an attempt to finally answer the question that emergency docs seem to have different answers to: will giving patients NSAIDs for their fracture-related pain actually lead to worse outcomes in terms of fracture healing?
Mechanism of action
NSAIDs work by inhibiting the COX enzyme that catalyzes the conversion of arachidonic acid into prostaglandins. In turn, prostaglandins work as inflammatory response mediators. When a bone is fractured, the healing process involves an inflammatory response. Giving NSAIDs alters that inflammatory response by decreasing prostaglandin production. This is why it’s been proposed that giving NSAIDs to patients with bone fractures will affect their healing.
Additionally, prostaglandins also modify the expression of bone morphogenic proteins (BMPs), which are involved in the bone healing process. This is another mechanism by which NSAIDs may affect fracture healing.
What the Research Shows
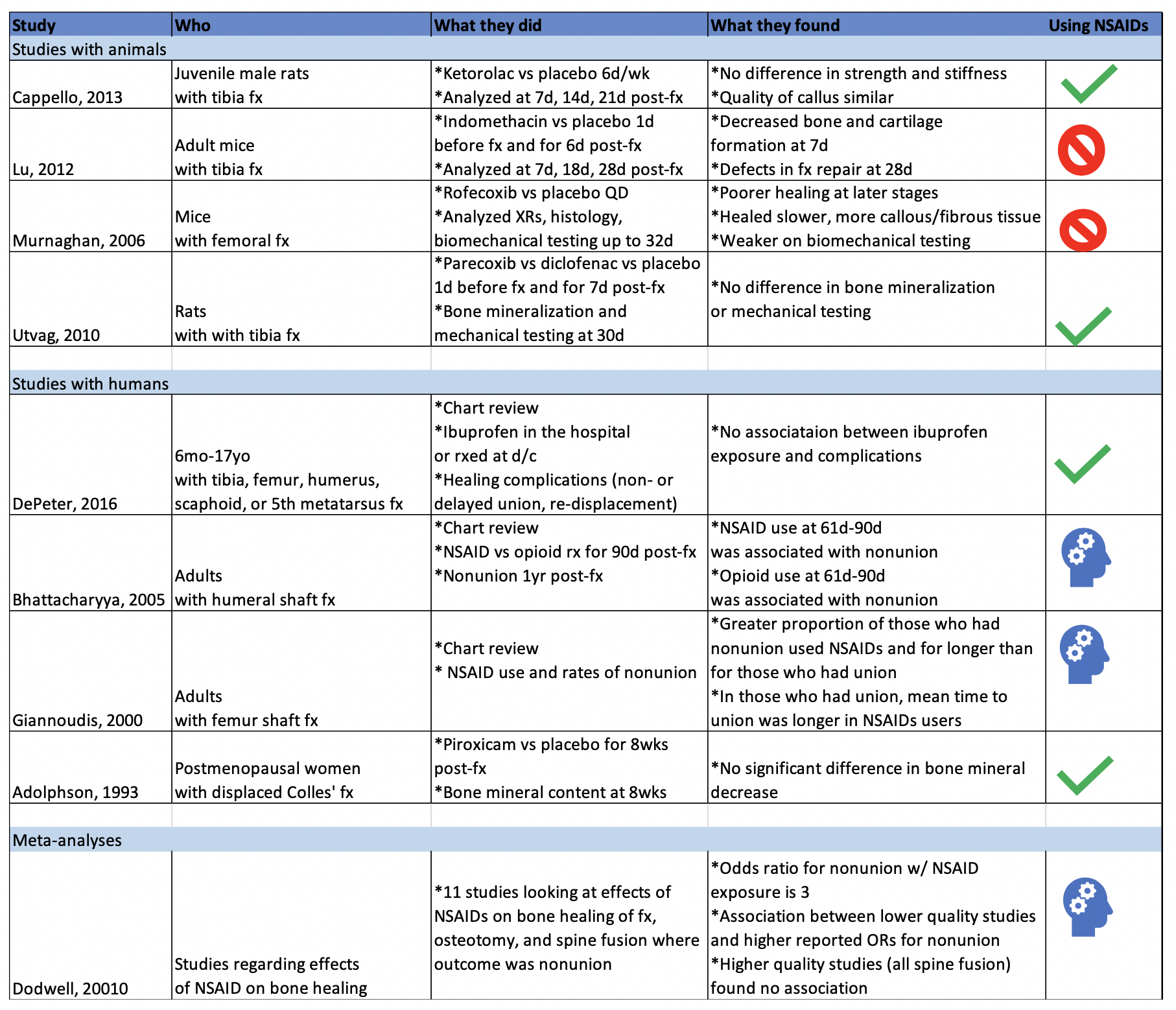
There have been a multitude of animal and human studies investigating the effect of NSAIDs on bone fracture healing, mostly in the orthopedic surgery community. The chart below has short summaries of some of the ones that are most relevant to emergency medicine.
Studies with Animals
Animal studies in general tend to use mice or rats with induced long bone fractures. The animals are exposed to NSAIDs or placebo and various bone characteristics are measured at various time frames. Capello, 2013 and Utvag, 2010 showed that Ketorolac, Parecoxib, and Diclofenac had no effect on strength, stiffness, or bone mineralization in rats with tibia fractures. On the other hand, Lu, 2012 and Murnaghan, 2006 showed that Indomethacin was associated with decreased bone and cartilage formation and that Rofecoxib was associated with slower and poorer healing in mice with tibia and femoral fractures, respectively.
Studies with Humans
While studies with animals have a lot of advantages, we’re often more interested in clinical outcomes than physiological nuances. DePeter 2016 in a retrospective chart review showed no association between ibuprofen exposure in kids with various fractures and healing complications like nonunion, delayed union, or re-displacement. However, there was no specification of the timeframe of treatment, and some patients received ibuprofen in the ED while others were sent home with it without a clear defined use period. Adolphson, 1993 showed there was no significant difference in bone mineral decrease in postmenopausal women with displaced Colles’ fractures that used Piroxicam for 8 weeks after the fracture compared to women who used a placebo. Giannoudis, 2000 found greater proportion of NSAID use in patients with nonunion of a femur shaft fracture compared to those who had union and found that in patients who had union, those who used NSAIDs took longer to achieve it. Bhattacharyya 2005 found that NSAID use at 61-90 days post fracture was associated with nonunion. However, an important thing to point out is that association does not equal causation. Is it that the NSAID use caused the poor outcome? Or is it that the poor outcome was more painful and thus those patients used pain medication for longer. To that point, Bhattacharyya, 2005 also found that there was an association between opioid use at 61-90 days and nonunion.
The Conclusion
The evidence isn’t slam-dunk in either direction on whether using NSAIDs impedes the fracture healing process. There aren’t many randomized control trials to explore causation (versus association) of NSAID use with fracture healing outcome. The one RCT I could find (Adolphson, 1993) leans towards no difference in outcome between NSAID users and placebo users. My takeaway: if my patients have no other contraindications to using NSAIDs and if their pain is well-controlled with said medication, then I’m going to advise they can use it for a short term and advise them to seek medical attention if they’re still needing to use NSADs regularly a few weeks out.
Expert Commentary
As is frequently the case in medicine, confounding factors make seemingly simple questions have not-so-simple answers.
Some animal studies suggested that NSAIDS can do harm to healing fractures. Others did not. The benefit of the animal study approach is that more variables can be controlled - the site of fracture, NSAID type, dose, frequency, duration of therapy. These animals were also surely more compliant with medications and follow up than our patients. However, animal studies do not necessarily translate to human outcomes. And these animal studies were less than definitive anyway.
The human studies were also less than definitive. Human studies are difficult for many reasons. Do NSAIDS affect pediatric, adult, elderly bone healing outcomes the same? Does it matter which NSAID, how often it is taken, the dose, the duration of use, which bone is fractured? When taking all these factors into consideration, it becomes more clear just how unclear the answer to this question is.
So at the end of the day, we do what we do time and time again in medical decision making – a risk-benefit analysis:
Option 1: Give NSAIDS. Risk causing an uncertain NSAID-related complication such as poor bone healing or a known NSAID complication such as a cardiovascular/GI/renal issue. Avoid narcotics.
Option 2: Give acetaminophen. Little downside as long as the patient can follow the directions you give them or on the bottle to avoid overdosing. Avoid NSAIDS and narcotics.
Option 3: Give narcotics. Avoid complications of NSAIDS. Expose to complications of narcotics. I don’t need to list these.
Option 4: Some combination of options 1, 2, and 3 because your gestalt is telling you that acetaminophen or NSAIDS alone won’t cut it for some cases.
I have different patients that end up falling into each of those options. This also raises another question - how do NSAIDS, acetaminophen, and opiates compare to each other for control of fracture pain? These scenarios and questions again demonstrate that medicine is often not a robotic one-size-fits-all, one-answer-to-every-question field, or else Dr. Google would replace us. Until more definitive RCTs come along, you will be required to use your judgment, or as I like to call it, expertise.
Matthew Levine, MD
Associate Professor
Department of Emergency Medicine
Northwestern University
How to Cite This Post
[Peer-Reviewed, Web Publication] Farcas A, Bode, J. (2020, April 6). Clinical Question: are we impeding our patients’ fracture healing by giving them NSAIDs? [NUEM Blog. Expert Commentary by Levine, M]. Retrieved from http://www.nuemblog.com/blog/fx-nsaids
Other Posts You Might Enjoy…
References
1. Adolphson, P., Abbaszadegan, H., Jonsson, U., Dalen, N., Sjoberg, H.E., Kalen, S. No effects of piroxicam on osteopenia and recovery after Colles’ fracture: A randomized, double-blind, placebo-controlled prospective trial. Archives of Orthopaedic and Trauma Surgery, 1993; 112: 127-130.
2. Bhattacharyya, T., Levin, R., Vrahas, M.S., Solomon, D.H. Nonsteroidal Antiinflammatory Drugs and Nonunion of Humeral Shaft Fractures. Arthritis & Rheumatism (Arthritis Care & Research), 2005; 53(3): 364-367.
3. Cappello, T., Nuelle, J.A.V., Katsantonis, N., Nauer, R.K., Lauing, K.L., Jagodzinski, J.E., Callaci, J.J. Ketorolac Administration Does Not Delay Early Fracture Healing in a Juvenile Rat Model: A Pilot Study. Journal of Pediatric Orthopaedics, 2013; 33(4): 415-421.
4. DePeter, K.C., Blumberg, S.M., Becker, S.D., Meltzer, J.A. Does the use of ibuprofen in children with extremity fractures increase their risk for bone healing complications? The Journal of Emergency Medicine, 2017; 52(4): 426-432.
5. Dodwell, E.R., Latorre, J.G., Parsini, E., Zwettler, E., Chandra, D., Mulpuri, K., Snyder, B. NSAID Exposure and Risk of Nonunion: A Meta-Analysis of Case-Control and Cohort studies. Calcific Tissue International, 2010; 87: 193-202.
6. Giannoudis, P.V., MacDonald, D.A., Matthews, S.J., Smith, R.M., Furlong, A.J., De Boer, P. Nonunion of the femoral diaphysis: the influence of reaming and non-steroidal anti-inflammatory drugs. The Journal of Bone & Joint Surgery, 2000; 82-B(5): 655-658.
7. Lu, C., Xing, Z., Wang, X., Mao, J., Marcucio, R.S., Miclau, T. Anti-inflammatory treatment increases angiogenesis during early fracture healing. Artchives of Orthopaedic and Trauma Surgery, 2012; 132: 1205-1213.
8. Murnaghan, M., Li, G., Marsh, D.R. Nonsteroidal Anti-Inflammatory Drug-Induced Fracture Nonunion: An Inhibition of Angiogenesis? The Journal of Bone and Joint Surgery, 2006; 88-A(3): 140-147.
9. Utvag, S.E., Fuskevag, O.M., Shegarfi, H., Reikeras, O. Short-Term Treatment with COX-2 Inhibitors Does Not Impair Fracture Healing. Journal of Investigative Surgery, 2010; 23: 257-261.
10. Yates, J.E., Shah, S.H., Blackwell, J.C. Do NSAIDs impede fracture healing? The Journal of Family Practice, 2011; 60(1):41-42.