Edited by: Maury Hajjar, MD (NUEM PGY-2), Niki Patel, MD (NUEM PGY-2), Vytas Karalius, MD, (NUEM PGY-2), Justine Ko (NUEM PGY-3) Expert commentary by: Seth Trueger, MD
Happy New Year, Everyone!
Let’s take a look back at the 2019 NUEM Blog!
The Top Ten NUEM Blog Posts of 2019
10. REBOA
Recent grads Andew Cunningham, Bill Burns, and Trauma/EM doc Zaffer Qasim walk us through the ever-popular and sublimely named REBOA.
9. The Seriousness of Deliriousness
Thorough discussion of the important but easy to overlook issue of delirium in the ED by Nery Porras, recent grad and current neuro critical care fellow Katie Colton and geriatrician Lee Lindquist.
8. Pelvic Fractures
Justine Ko, Terese Whipple, and Matt Levine walk is through pelvic fractures and the important associated injuries.
7. Verbal Deescalation in the ED
Vidya Eswaran, Zach Schmitz, Abiye Ibiebele, NUEM-blog-founder Michael Macias, recent grad Arthur Moore, and John Bailitz review the complex but important topic of verbal deescalation in the ED.
6. Visual Guide to Splinting
Recent grad and current Stanford med ed fellow, recentish grad John Sarwarkand remote grad Matthew Pirotte provide a surprising amount of information in a small amount of words & images.
5. Post-Intubation Management
It’s easy to fall into the trap getting the tube & high-fiving and walking away; Andra Farcas, recent grad and current Air Force doc Paul Trinquero and recentish grad Andrew Pirotte walk is through the steps to post-intubation management.
4. Flexor Tenosynovitis
Thorough and concise review of flexor tenosynovitis by Kevin Dyer and recent grad Adnan Hussain, featuring expert commentary hand surgeon Avi Giladi (who also had the #4 post in 2018).
3. Tetracaine
Nice review by Jonathan Hung and recent grad and current med ed fellow Matt Klein of an Annals study showing a safe approach to tetracaine for corneal abrasions. Won’t solve the controversy but does include an expert commentary by @DGlaucomflecken
2. Intubation Positioning: Beyond the Sniffing Position
Unfortunately, optimal positioning is not always optimally executed in the ED; this post reviews both “standard” sniffing position and ramping, which, if nothing else, will help push us to better position our patients. Very nice work by recent grad and current neuro critical care fellow Katie Colton, and recent grad Charles Caffrey, and recentish grad Andrew Pirotte!
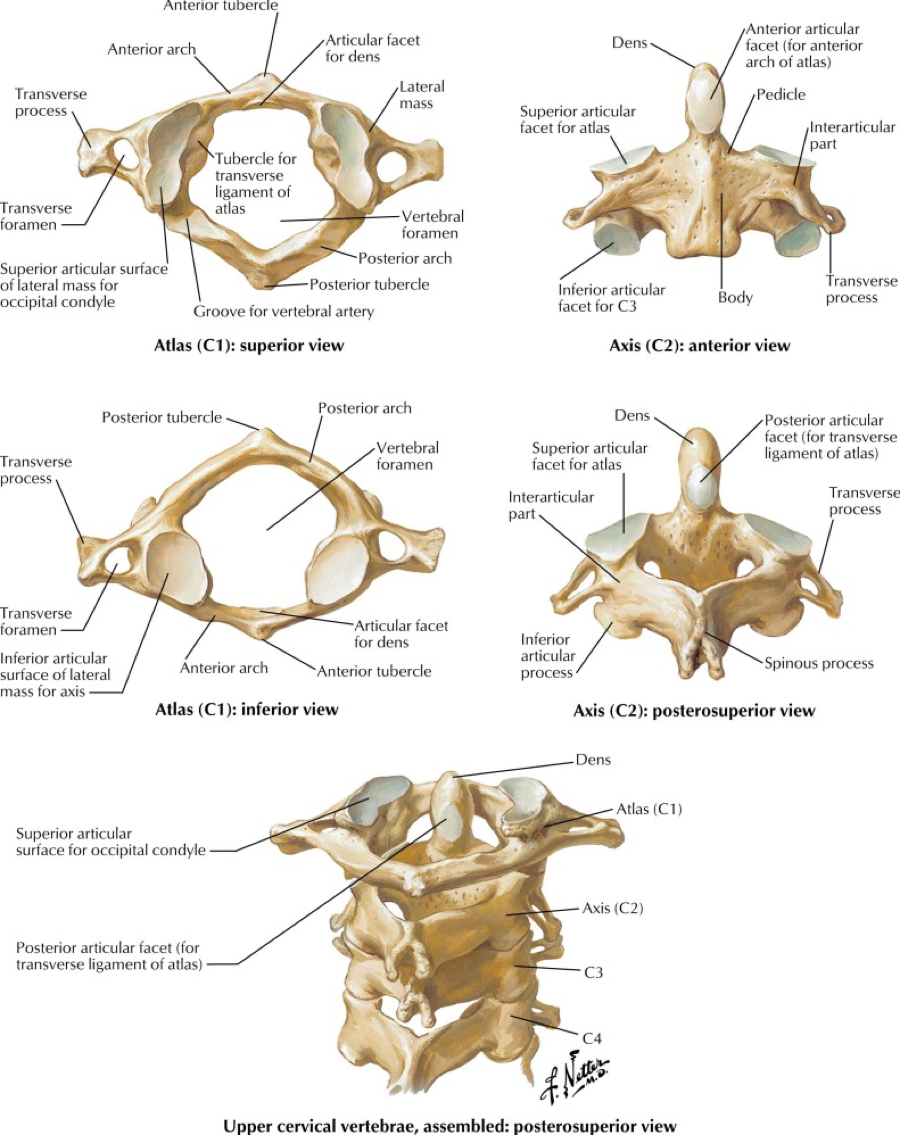
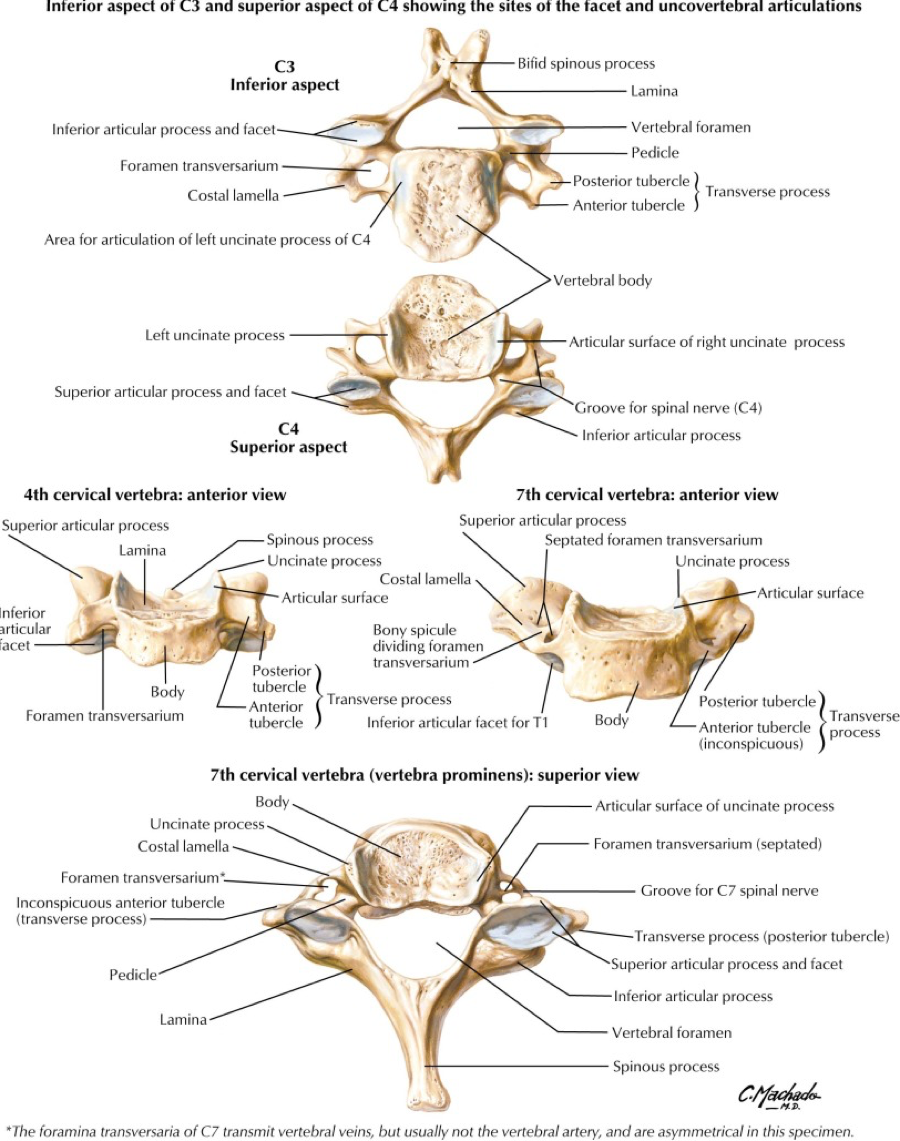
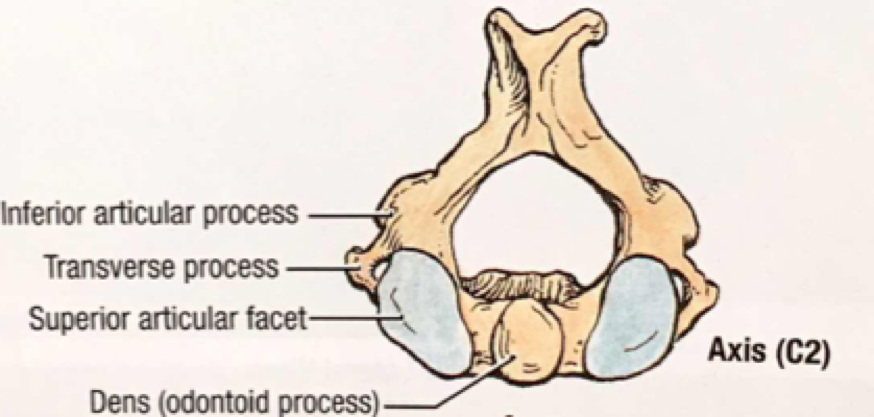
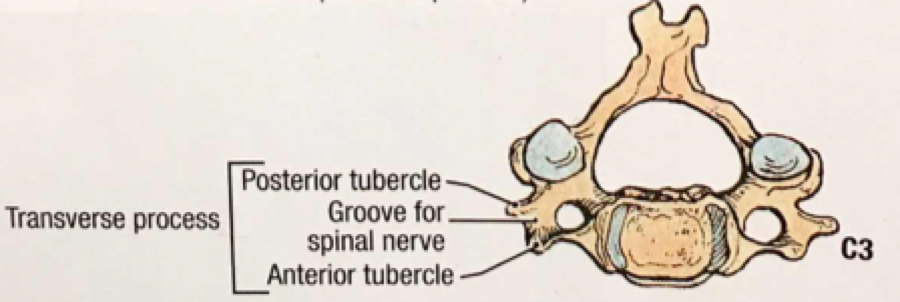
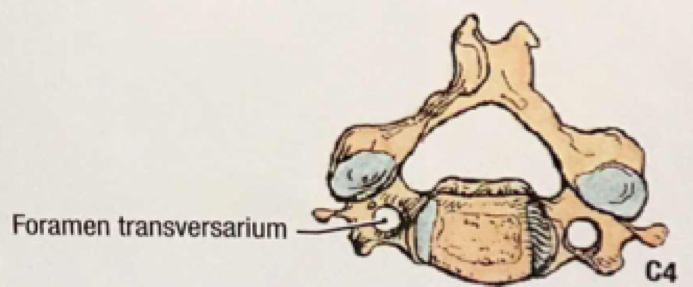
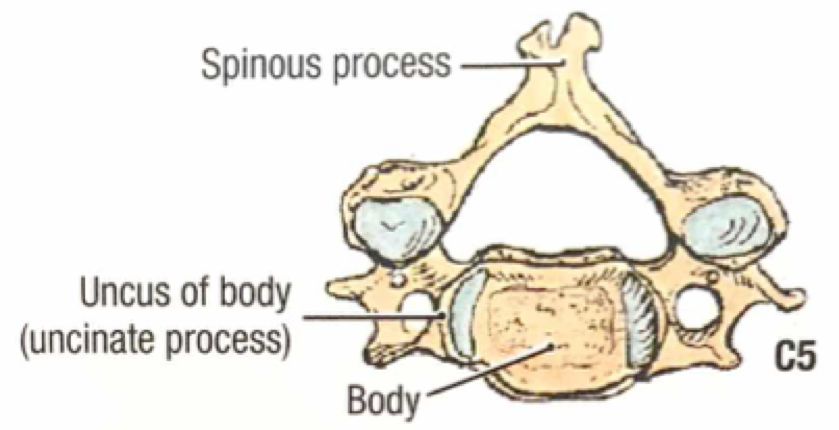
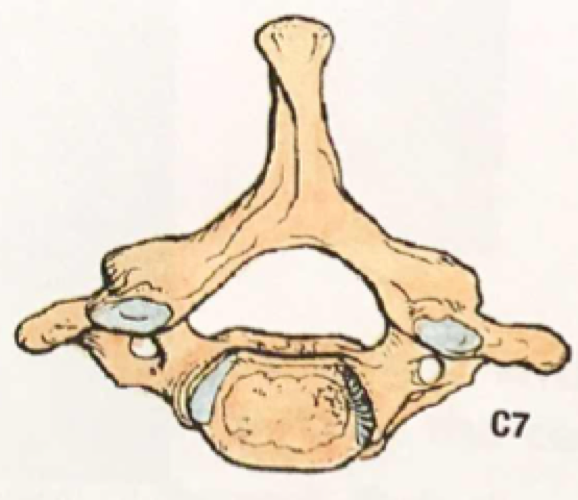
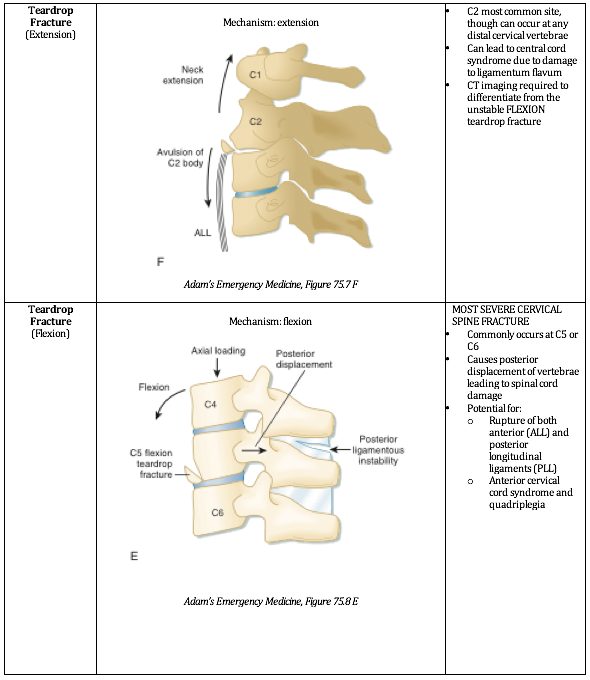
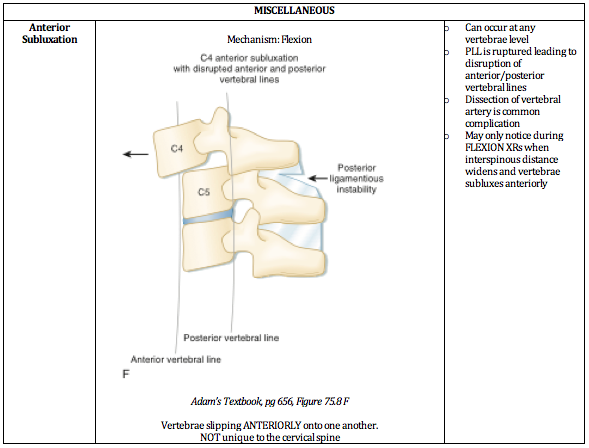
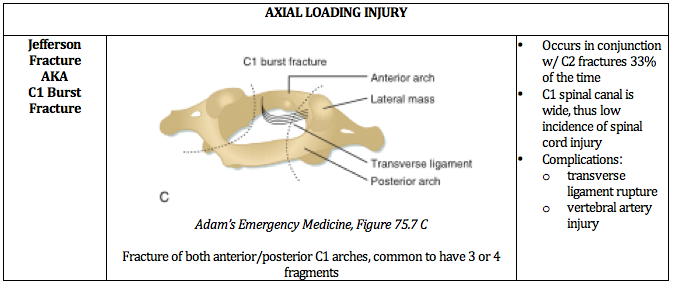
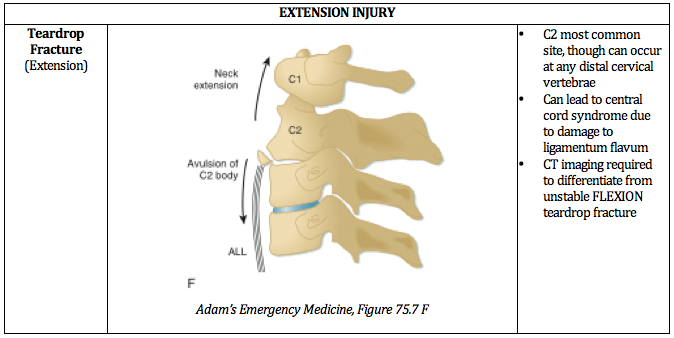
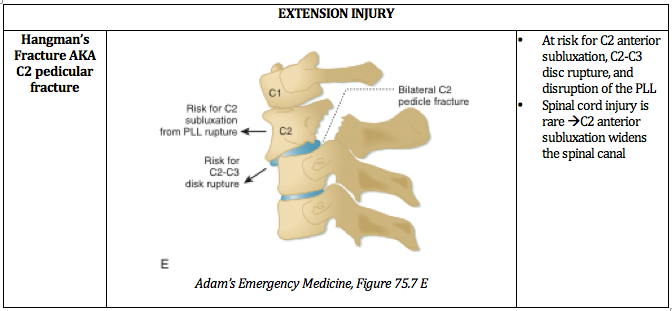
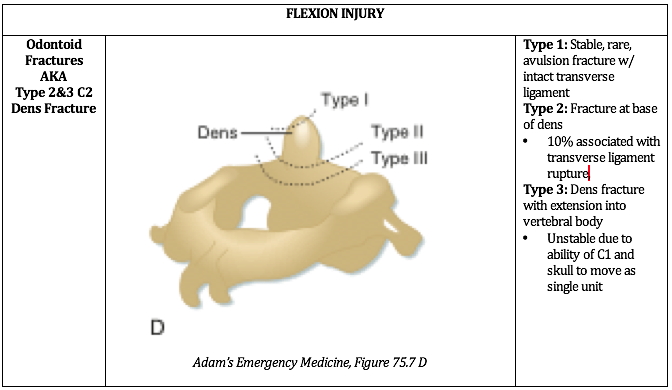
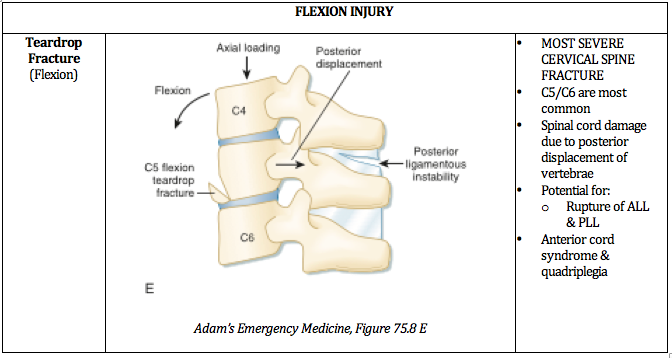
1. Unstable C-Spine Fractures
The top spot goes to a very nice succinct review by recent grads Sarah Sanders and Alison Marshall featuring beautiful images and a commentary by NLFH faculty Steve Hodges.
How to cite this post
[Peer-Reviewed, Web Publication] Hajjar M, Patel N, Karalius V, Ko J, (2019, December 30 ). The Top NUEM Blog Posts of 2019. [NUEM Blog. Expert Commentary by Trueger S ]. Retrieved from http://www.nuemblog.com/blog/top-ten-2019.